Update in clinical procedures
The quest for perfection. Achieving the best aesthetic results
Achieving the best aesthetic restorations: are materials the answer?
The speaker described the five-step treatment workflow which they use for all cases (fig 1):
- Determine the incisal edge position
- Depending on the complexity of the case, decide whether to change or maintain the maxilla–mandible relationship
- Choose the optimum vertical dimension for the case
- Restore the functional pathways (with anterior guidance)
- Provide posterior occlusal support to stabilise the aesthetic rehabilitation
Incisal edge position
The position of the incisal edge is determined by aesthetics (Ramfjord et al., 1966; Mohl et al., 1988; McNeill et al., 1997). The amount of tooth that is visible depends on the patient’s preference. It is also influenced by phonetics, since the incisal edge position affects the pronunciation of ‘S’ and ‘F-V’ sounds. Regarding function, this will be decided by the anterior limit of protrusive trajectory.
This position is determined with the ‘digital smile design’ app (DSD/APP). It is a useful tool to plan the rehabilitation, and to communicate with the patient about aesthetics through the use of pictures and dynamic recordings. To accurately judge the incisal edge position for each patient, it is vital to observe them smiling and talking in a video.
The 2D design has to be transformed into a 3D mock-up (whether from an analogical wax-up or a direct digital wax-up). The wax-up is used to fabricate the provisional, which can be printed or milled in the digital workflow. Once the provisional is approved, the definitive restoration can be made in any material – it is not the material that is the key to success, but the proper workflow.
Maxilla–mandible relationships
Next, a functional diagnosis is needed to see if patient’s occlusion should be changed. When the patient has a good balance between functional demands and their capacity to adapt (no complaints, no symptoms, and no signs of pathology or dysfunction), the occlusal scheme does not need to be changed. However, when the patient presents with temporomandibular joint (TMJ) or muscle pain, dysfunction, an uncomfortable bite, hypersensitive or worn teeth, broken restorations, abnormal tooth mobility, tooth migration, etc., we are likely facing pathologic occlusion. This occlusion must be re-organised in order to achieve the ideal model of therapeutic occlusion.
Centric relation
To re-organise occlusion, the start point should always be the centric relation, because it is a reproducible position (Keshvad & Winstanley, 2000-2001; Rinchuse & Kandasamy, 2006). There are numerous methods for achieving this, but the speaker highlighted Lucia’s jig (Lucia, 1964) and Kois’ de-programmer (Kois, 2002) methods as the two which are most convenient (in his experience) (fig 2–3). Both methods provide a stable first contact point position which can be scanned to prepare a highly accurate bite registration. A digital workflow allows us to avoid the errors which can arise in every step of analogue workflows.
Occlusal vertical dimension (OVD)
There is a great deal of misinformation about this topic. This is because, traditionally, it was recommended that OVD not be changed. However, in the majority of cases, OVD should be changed, as it provides several advantages (Calamita et al., 2019):
- allows more space for restorative material (attrition, enamel wear)
- can improve maxilla–mandible relationships (axial loads, overjet, overbite and angle of disclusion)
- opening the bite promotes aesthetic dento-facial harmony
Augmenting the OVD has been shown to be safe when it is made between the limits of the functional adaptation (McNeill et al., 1997; Abduo et al., 2012; Moreno-Hay & Okeson, 2015). When opening the bite, however, it should be noted that the occlusion has to be rebuilt in the three dimensions of the space (not just vertically). This has implications involving teeth, TMJs, muscles and phonetics. Therefore, to proceed, we must first work with provisionals. Provisionals at the same time act as a clinical test and as a guide for the definitive prosthesis.
How much OVD can be augmented? Posselt’s diagram shows that when the mandible opens, it also moves down and back (Posselt 1952). The ‘1-2-3 rule’ is a useful way to calculate this movement: for every additional 1mm in posterior teeth, the height in incisors increases by 2mm, the overjet by 1.3mm overjet and the incisal pin of the articulator by 3mm (Rebibo 2009) (fig 4).
The angle classification determines how much the bite opening should be increased. Class I bites can be opened easily. With class II, the lingual contact is lost when the bite is opened and the occlusion destabilises. In cases involving class III angles, the lingual position of the upper incisor can be compensated (if necessary) according to the treatment plan.
The literature tends to guide us towards opening the bite. Numerous methods have been described, like facial proportions, free-way space, deglutition, phonetics, cephalometric, cemento-enamel junction, occlusal splint or TENS.
The facial aesthetic harmony is not relevant in this process, since attempts to alter the height of the face by changing OVD by 2–6mm are not generally visible (Gross et al., 2002). However, it is sometimes the case that the facial height needs to be changed by at least 8mm, and with so large opening, the lingual face of the restorations will be too thick. This altered lingual incisor anatomy may cause phonetic alterations when pronouncing ‘S’ sounds.
Functional pathways
When lengthening the upper incisors, the anterior functional guidance should be considered to avoid hampering the mandibular displacement and overloading the restorations, which could lead to failure. The clinical relevance of this was proved in a study showing that the risk of veneer fracture is 2.3 times higher after incisal lengthening (Gurel et al., 2013). The flatter the disclusion angle, the less stress on the restorations (fig 5–6).
Posterior support
Digital tools which can register reference planes and scan dental arches may be used as an alternative to conventional articulators. Taking this even further, the speaker described some software that can scan the face and merge the CBCT records, to give us the so-called ‘digital patient’.[1]
Now, provisionals can be fabricated using several procedures. The speaker said they prefer the indirect bonded approach with polymethyl-methacrylate (PMMA), which can be either printed or milled, due to its strength and precise finish.
Treatment sequence
The sequence of the treatment move in the opposite direction to diagnosis (fig 7). After periodontal treatment, the old restorations are replaced with composite and the required endodontics are performed. Then, the single-unit PMMA additive provisionals are placed for aesthetic and functional test (fig 8). Next, the definitive restoration should start by placing using the lower anterior ceramic veneers, then lower posterior conservative crowns and onlays, and the upper anterior and posterior final restorations.
Materials
Provisionals are used as a guide for preparing the abutments for the final prosthesis. The speaker stated that they use leucite reinforced glass ceramic (Empress CAD®) in normal cases, as it offers the best combination of aesthetics and strength; in the case of bruxers, they use lithium disilicate (Magne & Belser, 2004; Gurel et al., 2005). Once all definitive restorations are cemented, it is time for occlusal equilibration and force control. To this end, different articulating papers are used, especially those with a thickness of 100, 21 and 8µ. Finally, a milled splint is placed and adjusted.
The speaker concluded by stating that perfection doesn’t exist. However, we can certainly get close to it with proper treatment planning and workflows, meticulous execution and a force control by occlusal equilibration.
[1] The speaker showed the Modjaw® software as an example.
Presentation figures
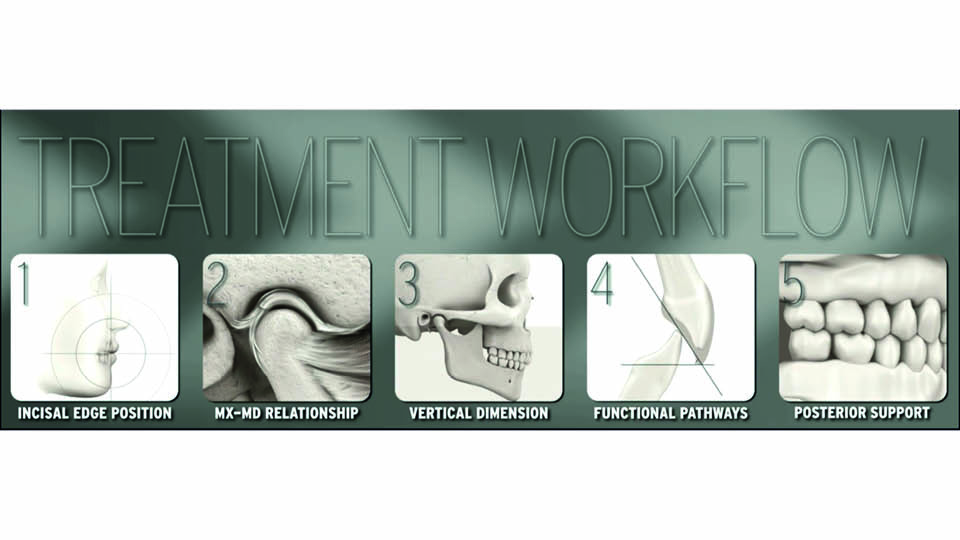
Fig 1: The five steps of treatment
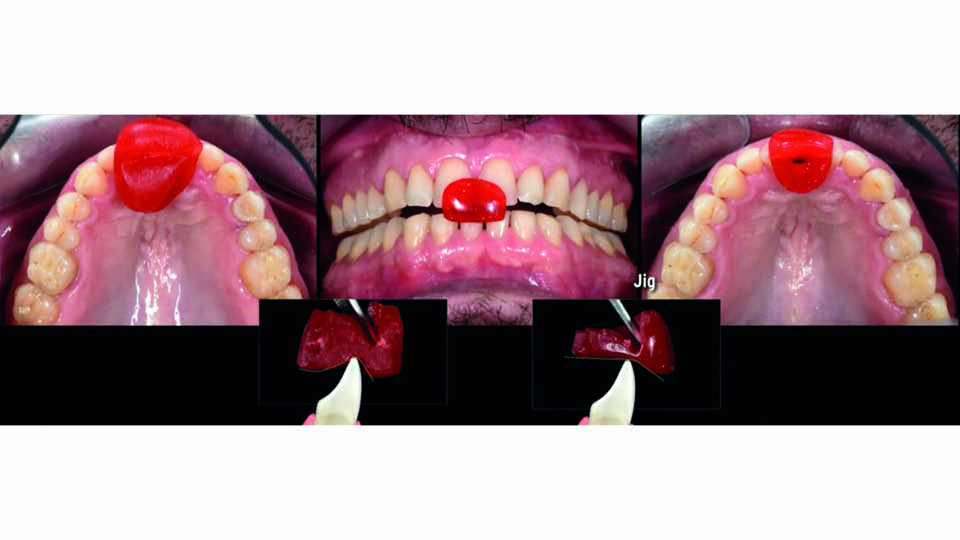
Fig 2: Centric relation: Lucia’s jig

Fig 3: Centric relation: Kois deprogrammer
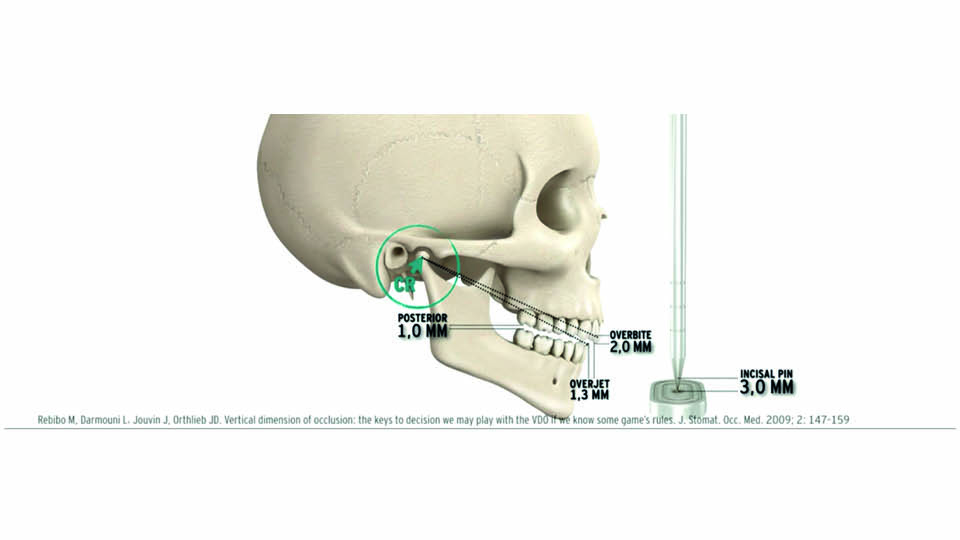
Fig 4: Vertical Dimension: the ‘1-2-3 rule’
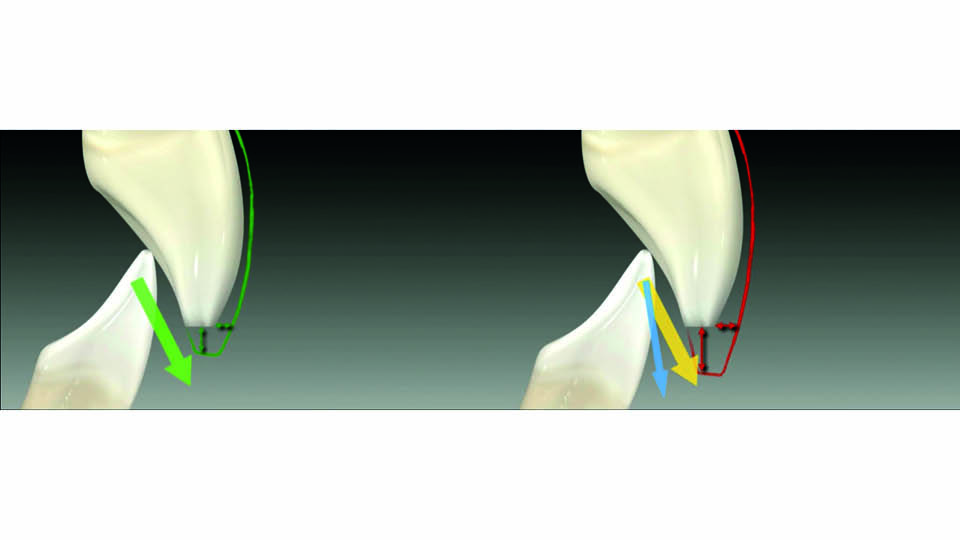
Fig 5
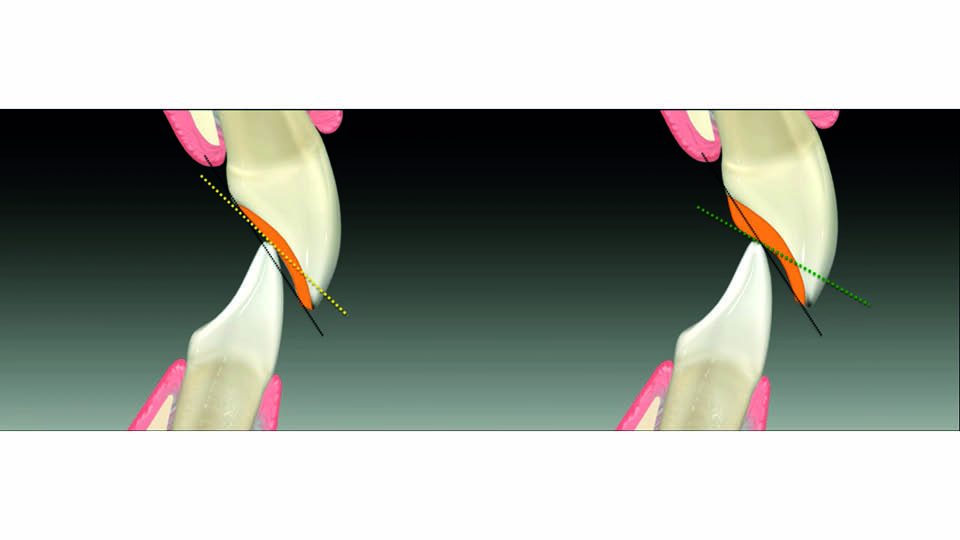
Fig 6

Fig 7: Treatment sequence
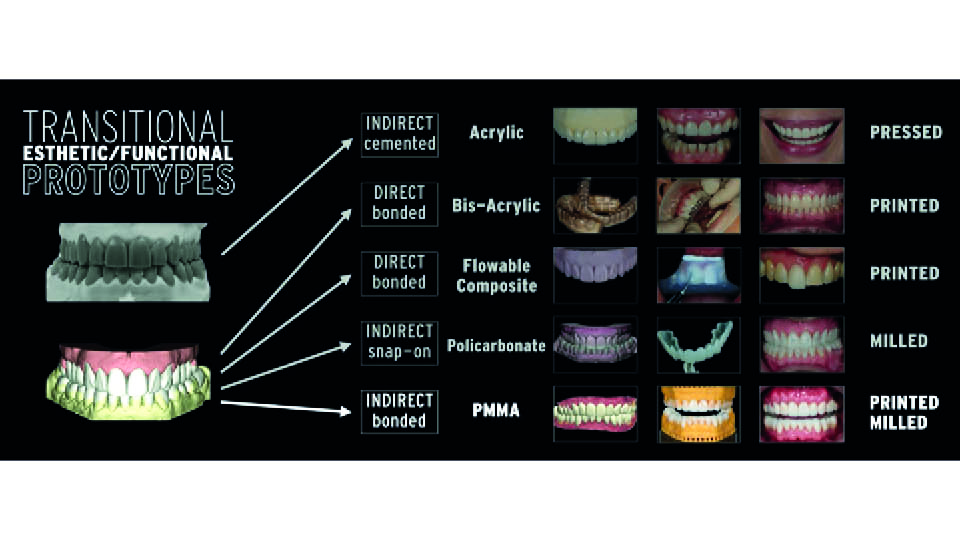
Fig 8: PMMA additive provisionals, the options
References:
Abduo J. Safety of increasing vertical dimension of occlusion: a systematic review. Quintessence Int 2012;43 (5):369-80.
Calamita M, Coachman C, Sesma N, Kois J. Occlusal vertical dimensión: treatment planning decisions and management considerations. Int J Esthet Dent 2019;14(2):166-81.
Gross MD, Nissan J, Ormianer Z, Dvori S, Shifman A: The effect of increasing occlusal vertical dimension on face height. Int J Prosthodont 2002;15(4):353-7.
Gurel G. The science & art of laminate veneers. Quintessence. 2005.
Gurel G, Sesma N, Calamita MA, Coachman C, Morimoto S. Influence of enamel preservation on failure rates of porcelain laminate veneers. Int J Periodontics Restorative Dent. 2013;;33(1):31-9.
Keshvad A. Winstanley RB. An Appraisal of the literature on centric relation. Part I. J Oral Rehabil 2000;27(10):823-33.
Keshvad A. Winstanley RB. An Appraisal of the literature on centric relation. Part II. J Oral Rehabil 2000;27(12):1013-23.
Keshvad A. Winstanley RB. An Appraisal of the literature on centric relation. Part III. J.Oral Rehabilt. 2001;28 (1):55-63.
Kois J. Occlusion: functional occlusion I. Course manual. Seattle, WA: 2002.
Lucia VO. Technique for recording centric relation. J Prosthet Dent 1964:14:492-505.
Magne P, Belser UC. Novel porcelain laminate preparation approach driven by a diagnostic mock-up. J Esthet Restor Dent 2004:16(1):7-16.
McNeill C. Fundamental treatment goals. In McNeill C et al. Science and Practice of occlusion. Carol Stream: Quintessence;1997
Mohl ND, Zarb GA, Carlsson GE, Rugh JD. A textbook on occlusion. Chicago. Quintessence;1988.
Moreno-Hay I, Okeson JP. Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral. Rehabil 2015:42:875-82.
Posselt U. Studies in the mobility of the human mandible. Acta Odonto Scand 1952
Ramfjord SP, Ash MM. Occlusion. Philadelphia: Saunders; 1966
Rebibo M, Darmouni L, Jouvin J, Othlieb JD. Vertical dimension of occlusion: The keys to decision we may play with the VDO if we know some game’s rules. J Stomat Occ Med 2009;2:147-59.
Rinchuse DJ, Kandasamy S. Centric relation: a historical and contemporary orthodontic perspective; J Am Dent Assoc 2006;137(4):494-501.
Prosthetic considerations when rehabilitating implants in the aesthetic zone
In the aesthetic area, four considerations are essential: form, colour, biocompatibility and mechanical performance. When considering aesthetics, perception is key. The patient’s perception is their subjective interpretation, and it should be carefully explored. An efficient and effective line of communication between the patient, dentist and technician is a prerequisite for good results. With this in mind, we must know which cases can compromise aesthetics over function, or function over aesthetics. The speaker presented three cases to illustrate these concepts (fig 9).
Case 1: congenitally missing upper lateral incisors
The patient wanted to replace their missing teeth. He had an average smile line, narrow restorative spaces, mild soft tissue volume deficiencies, an unfavourable canine relationship, increased vertical overlap and low value, high opacity teeth.
The first step is to prepare a wax-up and a mock-up to plan the aesthetic appearance and to guide implant surgery (fig 10). Provisional restorations guide the soft tissue by the critical and subcritical contours (Su et al., 2010) and the shape of the papilla by the position of contact points (Wittneben et al., 2013). The soft tissue profile is also influenced by times the number of times the abutment has been re-connected: the more disconnections, the more tissue is lost.
Material selection
Then, the supra- and infra-gingival shapes should be communicated to the lab and the material must be selected. Zirconia abutments can provide good aesthetic results (Brodbeck et al., 2003), but they are vulnerable to fatigue. Intraoral forces can break the abutments (Stimmelmayr et al, 2012, Klotz et al., 2011) or the implant platform may be damaged by the zirconia abutment (Kim 2013).
The alternative is to use zirconia-titanium in the abutment and a titanium-titanium connection between the abutment and implant platform (Guilherme et al., 2016). Although this option maintains the integrity of the implant platform, complications may still occur. Debonding of the titanium base or fracture (either of the titanium base or of the zirconia part) must be addressed by re-cementing the abutment base or replacing the whole abutment (Putra et al., 2019). Other biological complications may arise directly from veneered zirconia reconstructions cemented extraorally on non-original titanium bases. The significant increase in PD and BoP values observed in these cases may be due to the wide diameter and reduced height of the non-original bases (Asgeirsson et al., 2019).
Alternatively, whole titanium abutments can be chosen. These can also be gold coloured. It has been shown that patients do not perceive these abutments as unaesthetic (Bidra & Rungruanganunt, 2013). In this patient’s case, customised gold-coloured titanium abutments were used to prevent potential mechanical problems in the narrow spaces, and zirconia copings with ceramic crowns were cemented over them (fig 11–12).
To prevent the cement from flowing into the sulcus when the crown is inserted, a smaller copy of the abutment should be used (Wadhwani & Piñeyro, 2009).
Case 2: fractured upper central incisor
In this case, the fracture was in the crest level. Although controversial, the patient decided to extract the tooth and replace it with an implant. The coronal fragment of the tooth was attached with composite to a titanium cylinder and used as an immediate provisional (fig 13). To prepare the new provisional from the lab, a customised transfer was used to transmit the subgingival contour to the technician (fig 14). Additionally, pictures – normal and polarized – and videos of the patient smiling and talking were sent by email, and a telephone conversation was held to help explain the details. To perform the few changes required in the shape, a second provisional was made as an exact replica of the first one that was sent to the lab. The patient was travelling from Switzerland to Portugal and so there was limited clinical time with her available. By giving her a second provisional while maintaining the first one made out of the tooth fragment, the shade matching ability was improved. Cross-polarized pictures were also used, which can be very helpful for carrying out a virtual try-in of the final restoration. For this reason one single central incisor restoration was delivered in only one take. A virtual try-in was made before the definitive prosthesis was fabricated. The whole process demonstrates how difficult it is, and the effort required to achieve comprehensive communication with the technician in the quest for perfection.
The three disconnections in this case led to a degree of soft tissue volume loss, which has been established in the literature (Degidi et al., 2011; Grand et al., 2012; Koutouzis et al., 2017) (fig 15).
Case 3: acquired mucogingival deformities
The third case involved a young patient who wanted a pretty smile. They presented with missing soft tissues in 21–22 caused by periodontitis and a high smile line. Overcorrection by orthodontic extrusion was performed, and the surgical guide was then made to extract 21–22 and place two implants (fig 16–17). The early provisionals guided the cicatrisation; they looked good, but the patient didn’t like them because the teeth weren’t white enough and looked too wide. This feedback was communicated to the lab, and the veneers were cemented and new impressions of the two implants were sent with customised transfers. The final result was successfully accepted by the patient.
In summary
- form and colour are both important, but in the end the colour changes we perceive as dentists are not perceived by the majority of our patients if the remaining aesthetic parameters are met
- communication with the lab is of paramount importance
- the sub- and supra-gingival contours should be transferred
- videos with explanations can be more illustrative of the changes that need to be made in the laboratorial side, and polarised pictures make it easier to communicate exact colours
- we can compromise on aesthetics over function in cases involving colours low in value and high opacity teeth
- close attention must be paid to patients with a high smile line
- we can compromise on function over aesthetics when there is enough restorative space (both horizontal and vertically) and with aesthetically driven patients
Fig 18–19
Presentation figures

Fig 9: The three cases presented by the speaker

Fig 10: Case 1: Pre-surgical planning
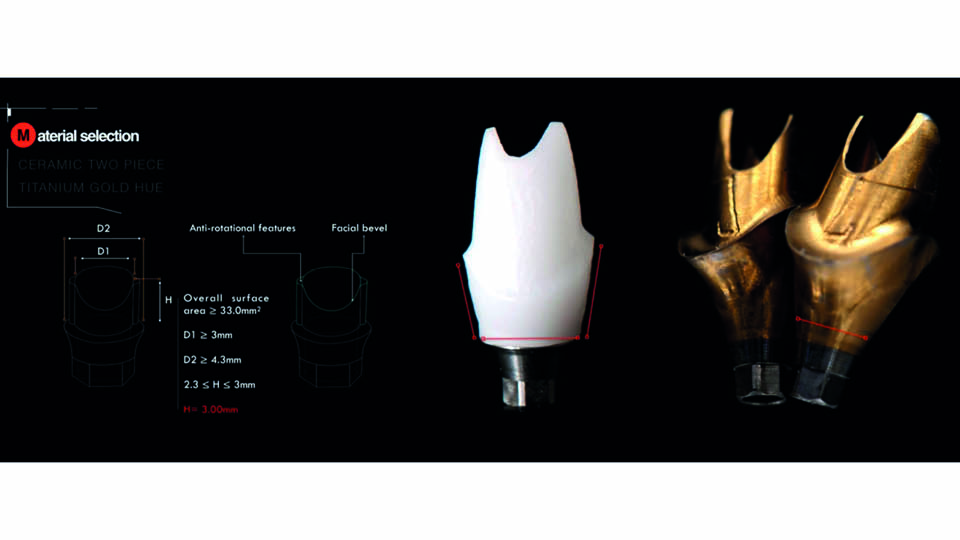
Fig 11: The gold-hue titanium abutments were selected

Fig 12: Zirconia copings and ceramic crowns

Fig 13: Case 2: fractured central incisor, pre- and post-surgery
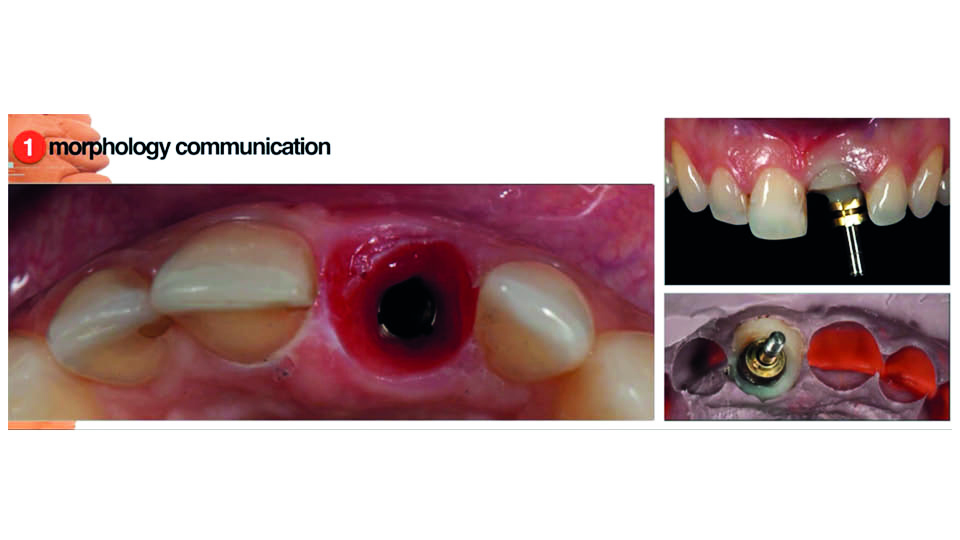
Fig 14
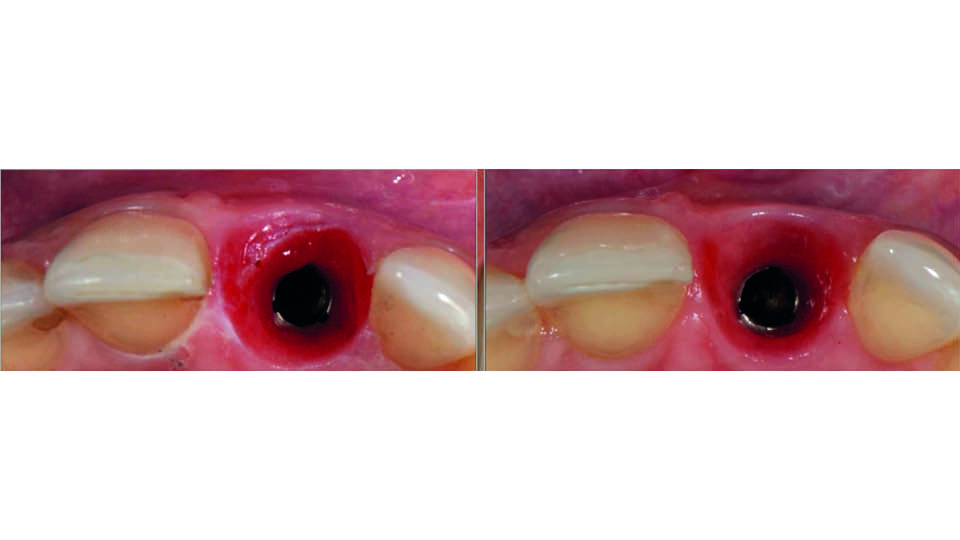
Fig 15: Tissue volume loss
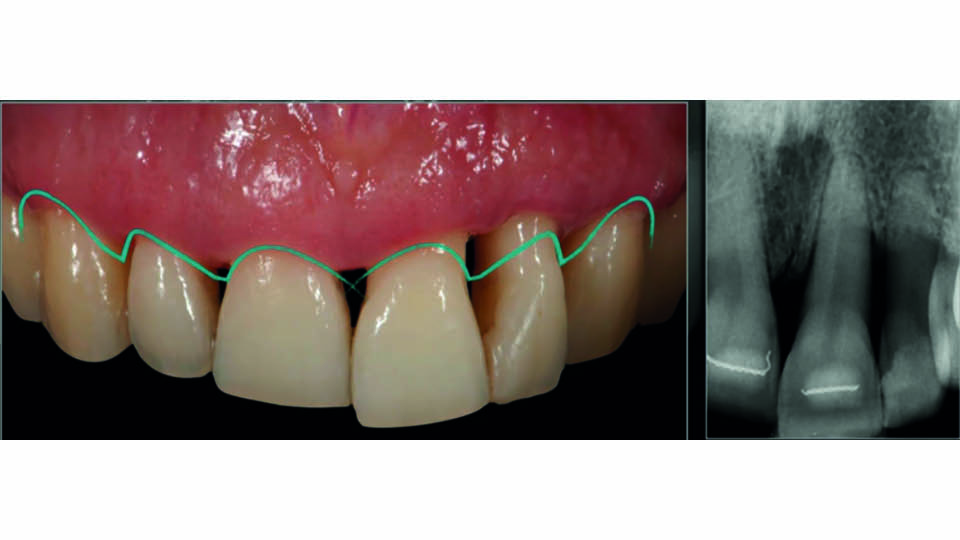
Fig 16: Case 3: Initial patient’s appearance
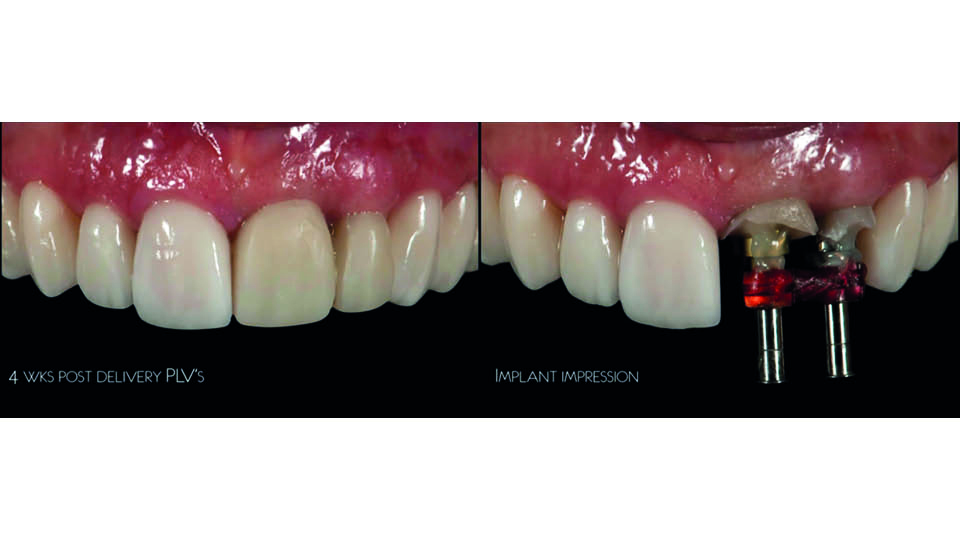
Fig 17: Treatment steps

Fig 18: Pre- and post-op pictures of the three cases presented

fig 19: Translucency of the final prostheses
References:
Asgeirsson AG, Sailer I, Gamper F, Jung RE, Hammerle CHF, Thoma DS. Veneered zirconia abutments cemented on non-original titanium bases: 1 year results of a prospective case series. Clin Oral Implants Res 2019;30(8):735-44.
Bidra AS, Rungruanganunt P. Clinical Outcomes of implant abutments in the anterior region: a systematic review. J Esthet Restor Dent 2013;25(3):159-76.
Brodbeck U: The ZiReal Post: A new ceramic implant abutment. J Esthet Restor Dent 2003;15(1):10-23.
Degidi M, Nardi D, Piatelli A. One abutment at one time: non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin Oral Implants Res 2011;22(11):1303-7.
Grand T, Guazzi P, Samarani R, Garuti G. Inmediate positioning of definitive abutments versus repeated abutment replacements in immediately loaded implants: effects on bone healing at the 1-year follow-up of a multi centre randomised controlled trial. Eur J oral Implantol 2012;5(1):9-16.
Guilherme NM, Chung KH, Flinn BD, Zheng C, Raigrodsky AJ. Assessment of reliability of CAD-CAM tooth-colored implant custom abutments. J Prosthet Dent 2016;116(2):206-13.
Kim JS, Raigrodski AJ, Flinn BD, Rubenstein JE, Chung KH, Mancl LA. In vitro assessment of three types of zirconia implant abutments under static load. J.Prosthet Dent 2013;109(4):255-63.
Klotz MW, Taylor TD, Goldberg AJ. Wear at the titanium-zirconia implant-abutment interface: a pilot study. Int J Oral Maxillofac Implants 2011;26(5):970-5.
Koutouzis T, Gholami F, Reynolds J, Kotsakis GA. Abutment disconnection/reconnection affects peri-implant marginal bone levels: a meta-analysis. Int J Oral Maxillofac Implants.2017;32(3);575-81.
Putra A, Chung KH, Guilherme NM, Cagna DR. Effect of bonding and rebonding on the shear bond strength of two-piece implant restorations. J Prosthodont 2019;28(3):305-9.
Stimmelmayr M, Edelhoff D, Guth JF, Erdelt K, Happe A, Beuer F. Wear at the titanium-titanium and the titanium-zirconia implant-abutment interface: a comparative in vitro study. Dent Mater 2012;28(12):1215-20.
Su H, González-Martín O, Weisgold A, Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int.J Periodontics Restorative Dent 2010;30(4):335-43.
Wadwani C, Piñeyro A. Technique for controlling the cement for an implant crown J Prosthet Dent 2009;102(1):57-8
Wittneben JG, Buser D, Belser UC, Bragger U. Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: the dynamic compression technique. Int J Periodontics Restorative Dent. 2013;33(4) 447-55.



