Dealing with complications
Biological and technical complications
Case 1: Large perforation of the sinus membrane during sinus augmentation
It has been reported that membrane perforations are the most frequently encountered surgical complication when performing sinus augmentation procedures. Small perforations can usually be successfully managed using resorbable membranes (fig 1). However, large perforations are difficult to treat (fig 2). According to the literature, when perforations are larger than 10mm, implant survival rate drops significantly, from 97 to 74% (Hernández-Alfaro et al., 2008).
The speaker described the sinus augmentation procedure, during which they encountered a large perforation (20x20mm) when lifting the membrane. It appears that membrane elevation is the most critical step of these procedures (Stacchi et al., 2015). The speaker reflected that an inadequate osteotomy design made the surgical access more challenging, and this may be what ultimately lead to the tear in the delicate Schneiderian membrane.
Conventional treatment guidelines dictate that we suture the membrane. However, this is a difficult procedure and in fact often results in the tearing of the membrane and new perforations. However, the speaker described the technique of making a hole in the lateral bony wall near the surgical window. The hole is used as a window through which to pull the membrane with a suture thread, and thus reduce the size needing to be covered with a collagen membrane. With this technique, there is no need to suture the perforation completely, thereby avoiding inadvertently causing additional damage to the Schneider membrane. Compared with the conventional procedure (suturing the two sides of the membrane), the bony hole reduces the tension and facilitates suturing (fig 3–4).
Presentation figures

Fig 1
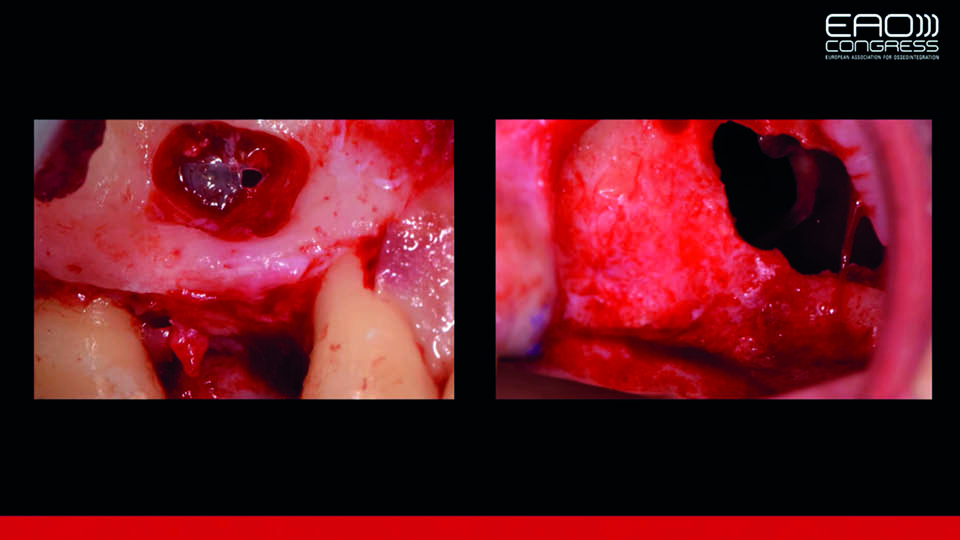
Fig 2: Small and large perforations
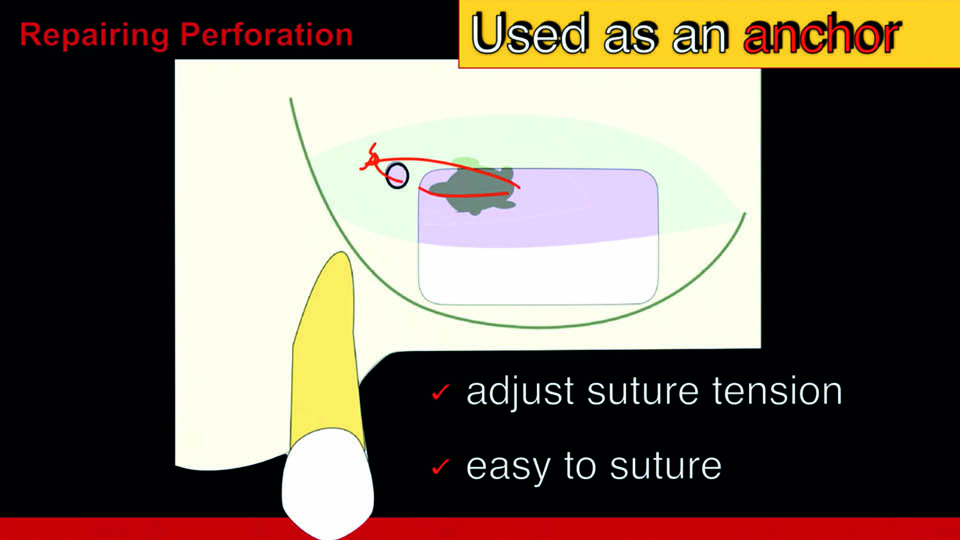
Fig 3: The technique presented
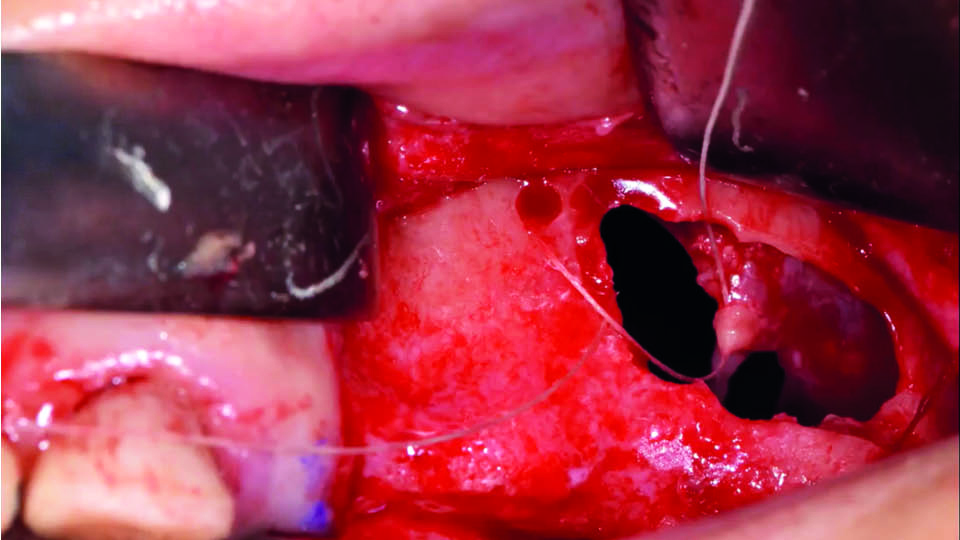
Fig 4: The technique presented
References:
Hernández-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implants Res 2008;19:91-8.
Stacchi C, Vercellotti T, Toschetti A, Speroni S, Salgarello S, Di Lenarda R. Intraoperative complications during sinus floor elevation using two different ultrasonic approaches: a two‐center, randomized, controlled clinical trial. Clin Implant Dent Rel Res 2015;17:e117-e125.
Vlassis JM & Fugazzotto PA. A classification system for sinus membrane perforations during augmentation procedures with options for repair. J Periodontol 1999;70(6):692-9.
Case 2. Ailing and failing implant associated with oroantral communication and endodontic lesions
The second speaker described a patient, who had presented with pain, fever and sinus suppuration along with oroantral communication and a 6mm vestibular bony dehiscence in a nearby implant (fig 5). Examination found multiple issues: possible bacterial contamination of the previous sinus graft, poor endodontic treatment and poor prosthetic treatment planning, all leading to biological failure (peri-implant bone loss and peri-implantitis) (fig 6).
It has been reported that sinus graft infection occurs in around 2.3% of all sinus grafting patients (Urban et al., 2012). The fist treatment objective was infection control. The failing implant at 16 was removed and pus was drained from the site. Simultaneously, the tooth at 15 was extracted and the peri-apical cyst was removed. The implant at 14 was kept (for the moment) to support a fixed temporary bridge along with a distal implant at the site of tooth 17. The root of 15 was then removed and granulation tissue was removed with thorough debridement. Six months later, re-entry was performed to place three more implants at 16, 15 and 14 with minor intra-alveolar sinus elevation. The implant showing buccal exposed threads was removed, and simultaneously a new implant was inserted. Guided Bone Regeneration with resorbable collagen membrane and a mixture of autologous bone and demineralized bovine bone was executed on the implant at 14. Simultaneous GBR was performed in 15, and all implants were immediately loaded with a new fixed provisional (fig 7–8). No connective tissue graft was required and prosthodontic treatment continued uneventfully. The speaker shared their four-year follow-up (fig 9–10).
Presentation figures
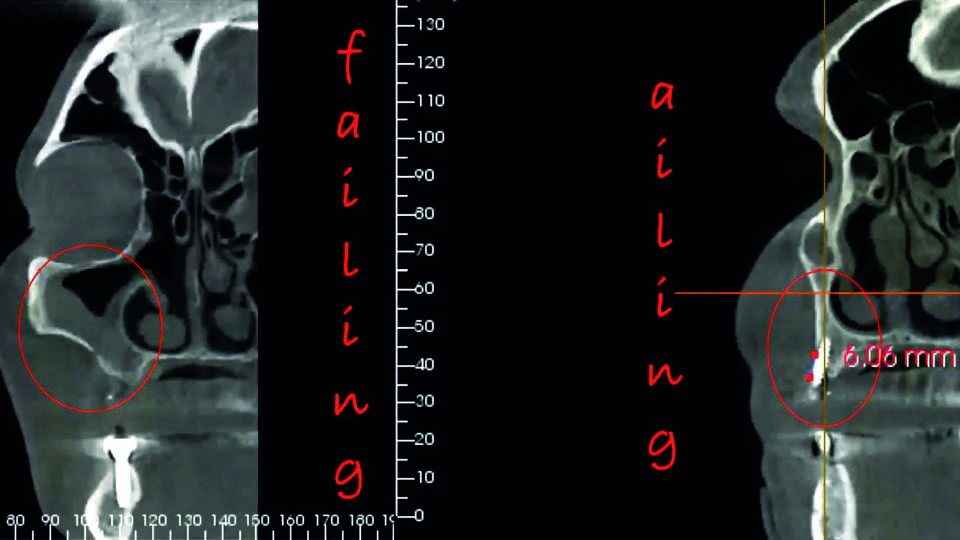
Fig 5
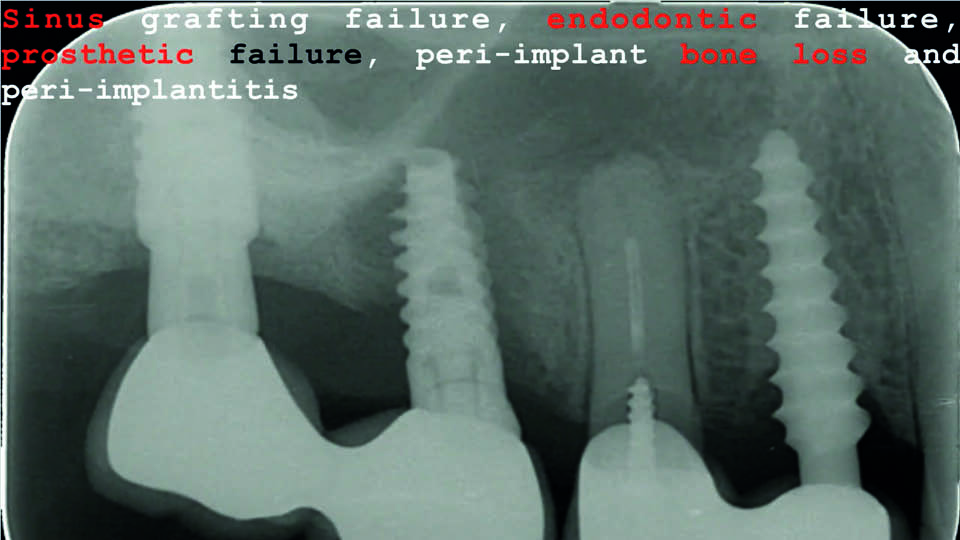
Fig 6
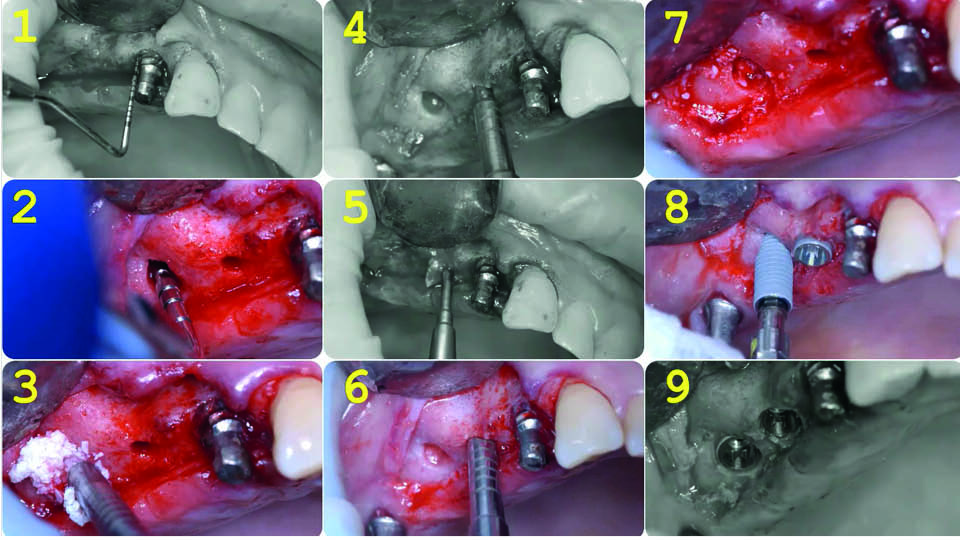
Fig 7: Treatment sequence
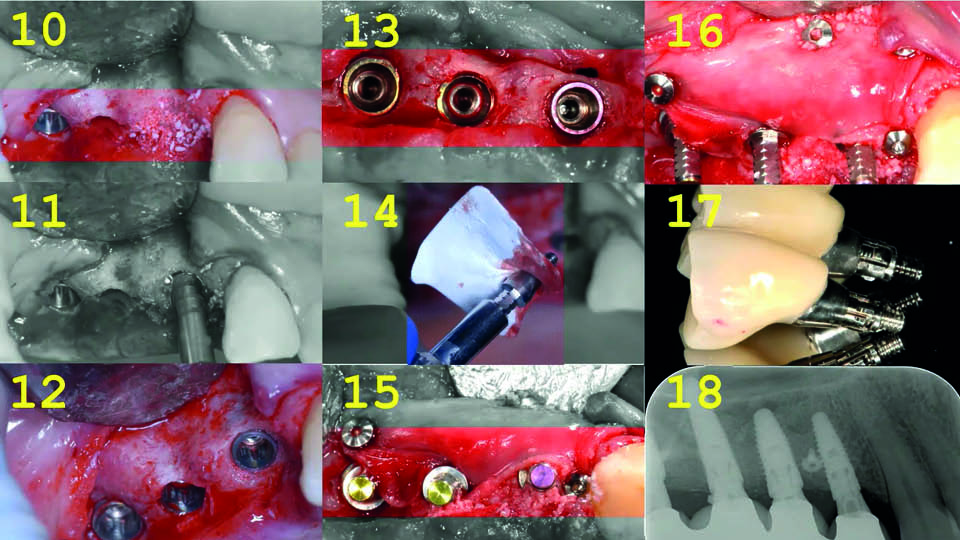
Fig 8: Treatment sequence
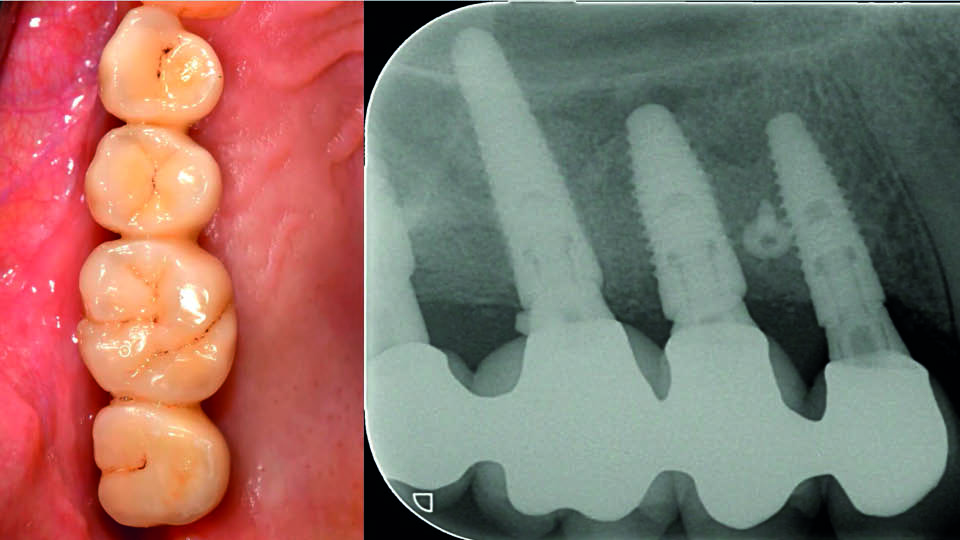
Fig 9: The four-year follow-up

Fig 10: The four-year follow-up
References:
Urban IA., Nagursky H, Church C, Lozada JL. Incidence, diagnosis, and treatment of sinus graft infection after sinus floor elevation: a clinical study. Int J Oral Maxillofac Implants, 2012;27(2):449-57.
Case 3. Failure of allogenic block graft
The next case involved a twenty-year-old patient with missing anterior teeth due to a car accident. The patient had hard and soft tissue deficiencies in the upper anterior region.
The speaker outlined a four-stage treatment plan:
- Allogenous bone block graft in the maxillary frontal area combined with GBR using Bio-oss® and Bioguide®. Temporisation achieved with an Essex appliance (in place until stage 3)
- After 6–7 months, placement of two two-piece implants with rough surfaces
- After 4–6 months, fabrication of a three-unit fixed provisional prosthesis
- After 2–4 weeks, delivery of the final zirconia bridge
The operation was performed according to current treatment guidelines, and each step is outlined in figures 11–14.
Healing was uneventful, although a lack of attached gingiva and a decrease in vestibular depth were observed in the area (as would be expected). The six-month post-op CBCT showed a gap between the bony bed and the block graft. When reopening, most of the bone block had become granulated tissue and no ossification was present.
Reflecting on this outcome, the speaker stated that the following factors may have been reasons for failure:
- the inadequate amount of keratinised gingiva should have been corrected before the block grafting was planned
- a combination of improper fit between the block and recipient bed, insufficient number of screws to prevent micromovement and excessive thickness of the blocks used
- there may have been pressure exerted over the graft during function with mobile soft tissues
- an autogenous bone block could have produced better results than an allogenic block
- the graft may have been infected
A vestibuloplasty using Mucograft® was then performed (fig 15–16). An autogenous bone block is planned, after which the original prosthetic treatment plan will be carried out.
Presentation figures
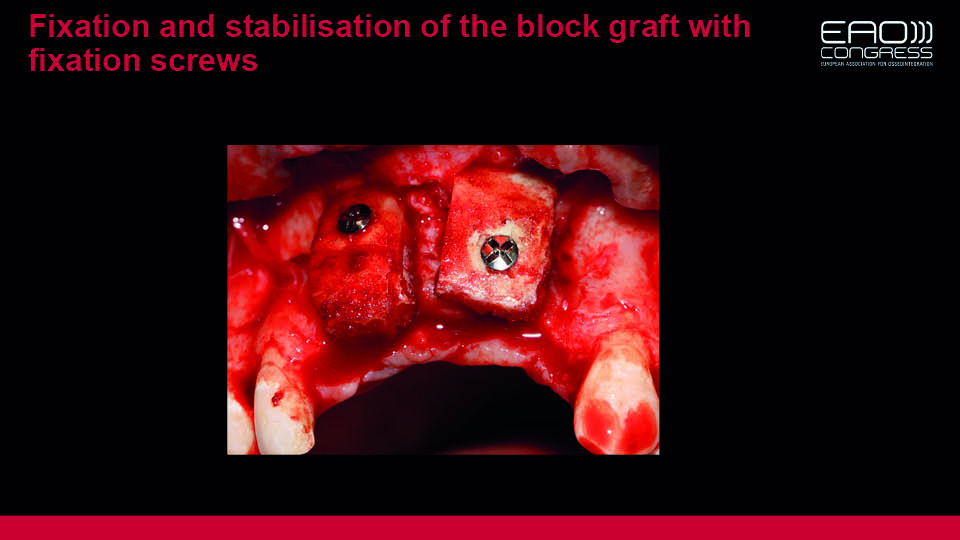
Fig 11
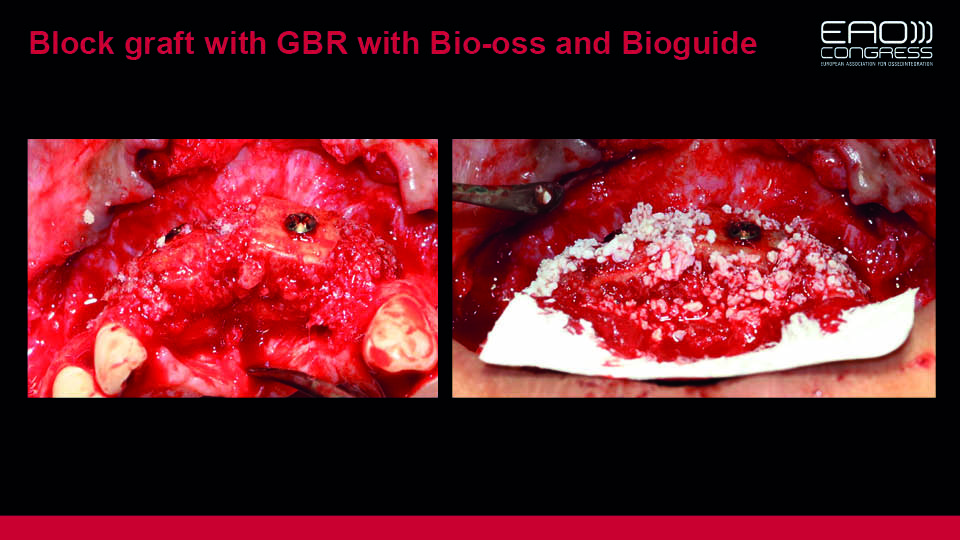
Fig 12
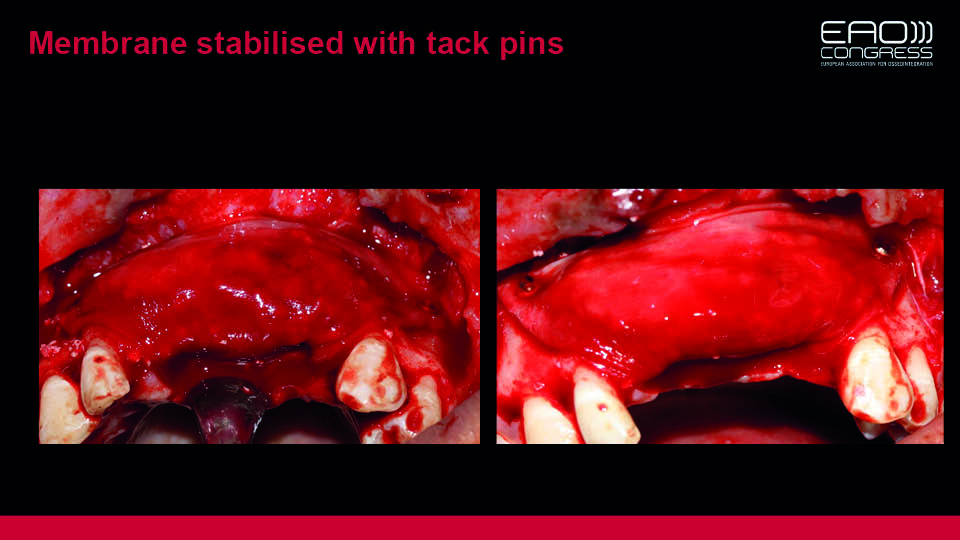
Fig 13

Fig 14
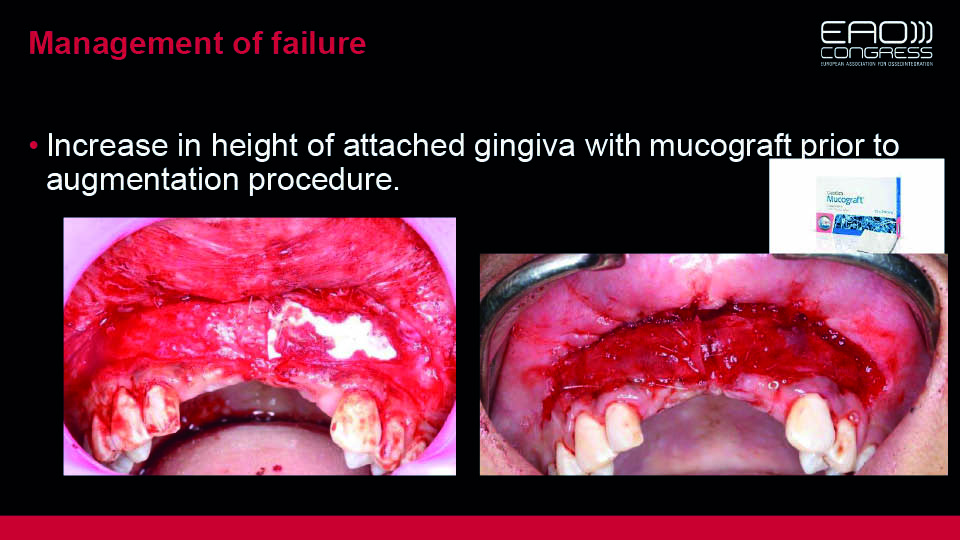
Fig 15

Fig 16
Case 4. Dental pathology contributing to implant failure
The speaker presented the case of a 55-year-old patient, complaining of pain and swelling at tooth 12 (which had previously received root canal treatment and apiceptomy in 1998). Then, in 2007, an implant had been placed at tooth 11. Now, percussion testing on tooth 12 was positive and a probing depth of 9mm was measured between teeth 12 and 11. Imaging confirmed both peri-implant infection and apical pathology of tooth 12. A surgical approach was undertaken in an attempt to debride the peri-implant defect and to revise the previous apicectomy – this revealed a communication between the apical area of the tooth and the distal and apical defect of the implant.
The prevalence of apical lesions around implants has been estimated to be around 0.3 to 8.2%. When implants are used to replace teeth which have previously had periapical lesions and/or been endodontically treated, the prevalence of these lesions increases to nearly 14%. Furthermore, when adjacent teeth have periapical lesions, the reported prevalence can reach 25%. However, since the aetiology is multifactorial, no consensus can be found in the literature regarding treatment.
According to the recommended decision-making flowchart devised by Chan et al. (2011) (fig 17), surgical intervention was planned in order to:
- access and debride the peri-implant lesion
- decontaminate the implant surface
- graft the defect
- eliminate the associated periapical pathology by performing a new apiceptomy
However, the surgical sites failed to heal and the patient continued to complain of local inflammation and pain. The decision was then made to remove the implant and the tooth. A free gingival graft was placed on the socket and a fixed bridge was planned to replace the missing teeth. The speaker stated that to avoid these types of complications when placing implants, the presence of neighbouring periapical lesions should be taken into account as sources of bacterial contamination. The extraction socket should be thoroughly curetted in order to eliminate granulation tissue, and longer healing periods should be observed following endodontic treatments.
The speaker stated that to prevent this complication when placing implants, the presence of neighbouring periapical lesions should be taken into account as sources of bacterial contamination. The extraction socket should be thoroughly curetted in order to eliminate granulated tissue, and a longer healing period should be observed after endodontic treatments. Maintenance is key to control this kind of problem from the beginning.
Presentation figures
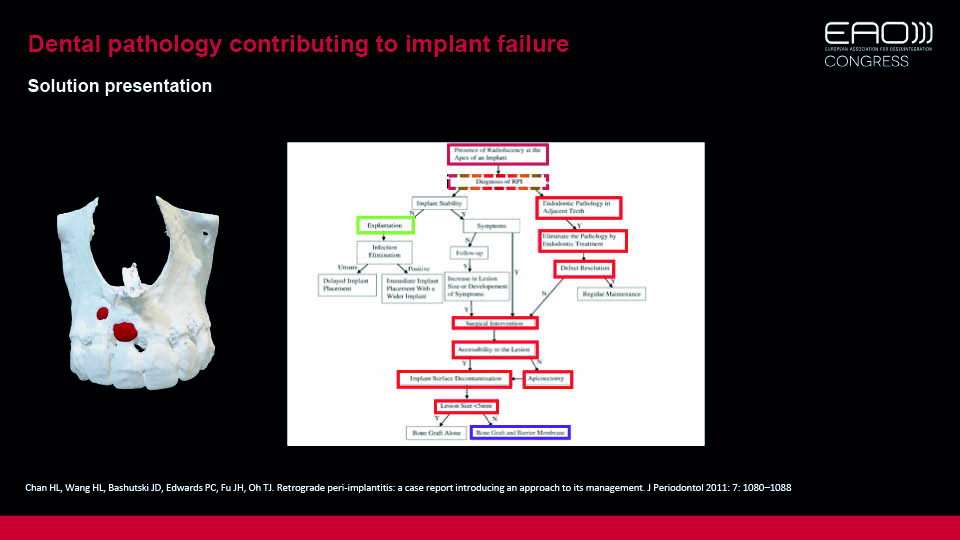
Fig 17: A decision-tree
References:
Dahlin C, Nikfarid H, Alsén B, Kashani H. Apical peri‐implantitis: Possible predisposing factors, case reports, and surgical treatment suggestions. Clin Implant Dent Rel Res 2009;11(3):222-7.
Chan HL, Wang HL, Bashutski JD, Edwards PC, Fu JH, Oh TJ. c. J Periodontol 2011;82(7):1080-8.
Temmerman A, Lefever D, Teughels W, Balshi TJ, Balshi SF, Quirynen M. Etiology and treatment of periapical lesions around dental implants. Periodontology 2000, 2014;66(1):247-54.
Case 5. Complications and management of All-on-4 treatment – a case report
The next speaker presented their case report involving a 55-year-old male patient who had a terminal dentition, with multiple teeth lost due to periodontitis. The patient was a heavy smoker, and wanted a fixed reconstruction. To this end, four implants in the maxilla and six in the mandible were planned. Surgical guides were prepared and implants were placed as part of a flapless approach. Next, impressions were taken and a provisional prosthesis was installed in 24 hours.
Eight months later, biomechanical complications began to appear in the maxillary all-on-4 reconstruction. The distal implant’s osseointegration had been lost; the abutment of the implant in the right central incisor had fractured; the prosthesis had broken in the right premolar area and the corresponding implant showed signs of bone resorption (fig 18–19). Since these complications were all signs of overloading, the option of re-placing the lost implant to restore the all-on-4 reconstruction was rejected. Instead, the decision was made to increase the number of implants in the maxilla. Approximately one year later, the final restoration was placed (fig 20–21).
The speaker concluded by analysing the potential reasons for these complications. They were classified as:
- patient factors: smoking, poor oral hygiene, history of periodontitis, bruxism
- surgical factors: an all-on-4 protocol was selected to simplify the treatment without bone augmentation procedures; however, only four implants in the maxilla proved to be insufficient to compete with six in the mandible
- prosthetic protocol: the use of cantilevers in temporary dentures may have contributed to extra forces against the implants and represented the weakest points
Presentation figures
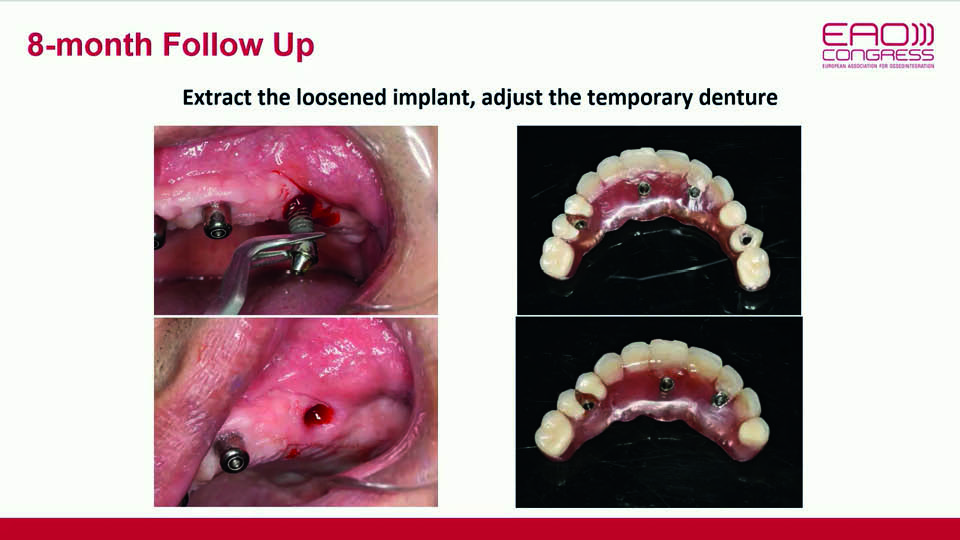
Fig 18
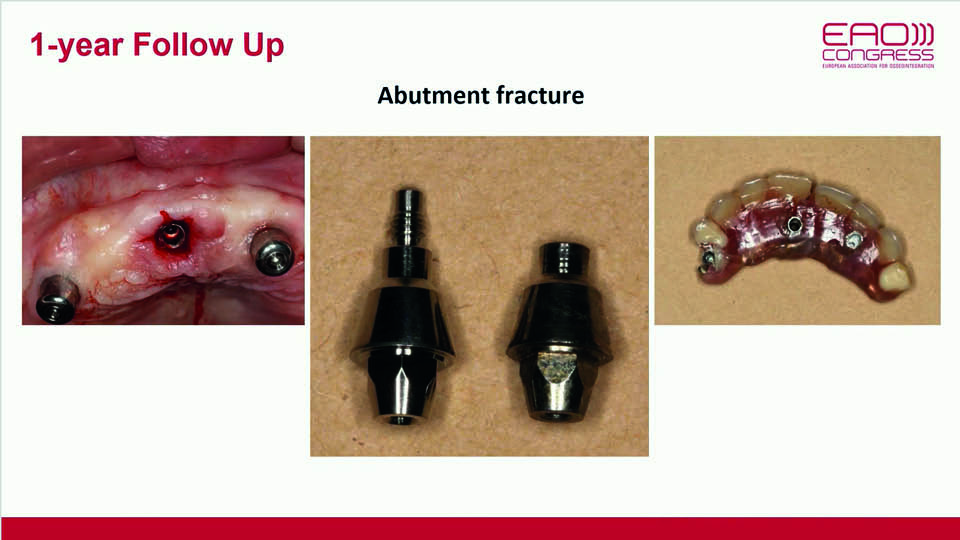
Fig 19
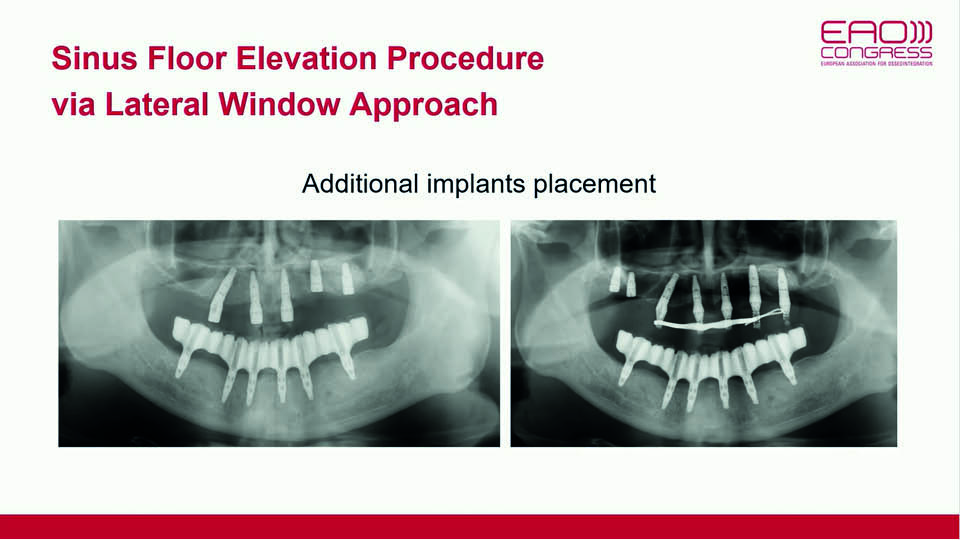
Fig 20
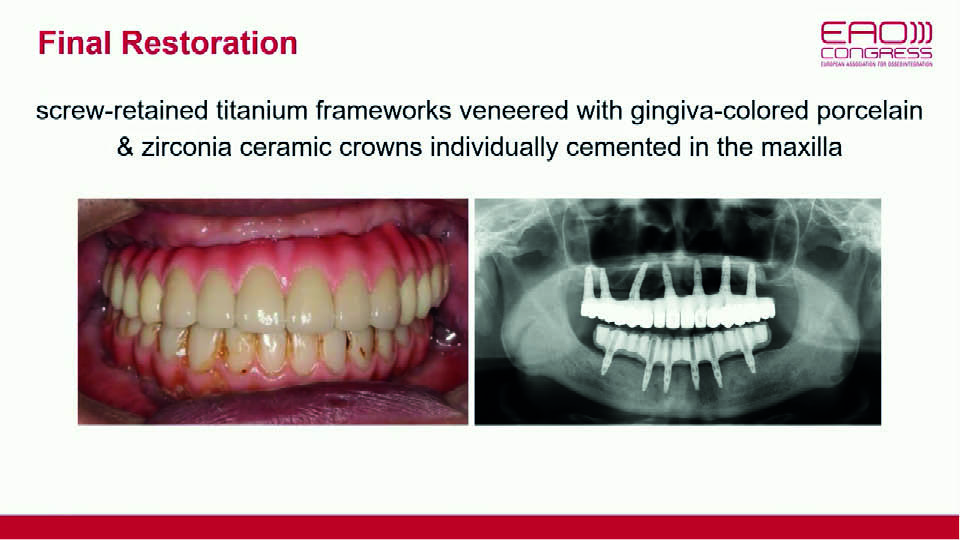
Fig 21
Case 6. Surgical treatment outcome of crestal bone loss of dental implant with Er:Yag laser – a case follow-up
The final case presented involved a 52-year-old woman who was referred to the clinic to have two implants placed (to replace missing left mandibular molars). Two months after surgery, significant crestal bone loss was observed. There are multiple factors which could have been the cause (Oh et al., 2002).
The approach selected to combat this involved decontaminating the surface in order to promote re-osseointegration (Mellado-Valero et al., 2013). An Er:Yag laser was used, and the area was then grafted. Two months later, the peri-implant bone had regenerated and prosthetic treatment was completed.
Main concepts presented and evidence
- early crestal bone loss around implants is often greater during the healing period and first year of function than the bone loss that occurs in the following years (evidence type I: RCT)
- one of the key ways to prevent early bone loss is by controlling insertion torque (evidence type III: clinical experience)
- the Er:Yag laser only demonstrated slight advantages for intraoral bone grafting procedures. Combined therapy may provide an effective treatment approach for peri-implant disease (evidence type II: prospective studies)
References:
Mellado-Valero A, Buitrago-Vera P, Solá-Ruiz MF, Ferrer-García JC. Decontamination of dental implant surface in peri-implantitis treatment: A literature review. Med Oral Patol Oral Cir Bucal 2013;18 (6):e869-76.
Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science?. J Periodontol 2002;73(3):322-33.



