Update in clinical procedures
How to treat cases involving buccal bone loss after extraction
The IDR (immediate dentoalveolar restoration) solution
The speaker clearly stated that he recommends treating fresh extraction compromised sockets with a single flapless procedure. The aim with this approach is to preserve and, at the same time, regenerate the natural biology of surrounding tissues. In the speaker’s experience, this approach is less invasive, and is shorter and less expensive than the conventional delayed approach. Above all, it can provide more predictable results.
The immediate dentoalveolar restoration (IDR) solution can be used in cases involving compromised alveolar sockets. It is a minimally invasive technique of grafting with bone, which eventually also uses soft tissue in it at the same time (not later), taken from the tuberosity at the time of implant placement. A portion of cortico-cancellous bone is removed from the tuberosity and placed as a membrane covering some particulate autogenous bone to restore the buccal bony wall and the lost volume (fig 1–2).
It has been well documented that the procedure can achieve long-term maintenance of the new buccal bone volume (Rosa et al., 2014; Rosa et al., 2016). The height of restored papillae have also been shown to remain stable, preventing subsequent marginal recessions.
As part of the procedure, it is recommended that the implant is placed palatally (after having been planned by a CBCT). The speaker said there should be 3mm between the implant shoulder and the gingiva on the buccal side. If there is 3mm of bone at the buccal aspect, a soft tissue graft to compensate won’t be needed.
When harvesting the bone graft from the tuberosity, the chisel should be angled perpendicular to the bone wall (or as much as is possible). As soon as the chisel goes deeper, the angulation should be adjusted progressively. The graft can then be reshaped according to the defect configuration and placed 1mm coronally to the implant position. The gap between the implant and the cortico-cancellous shield is filled with particulated bone also obtained from the tuberosity. An immediate temporary crown is finally screwed onto the implant without occlusion. A 2mm gap should be left to allow the soft tissue to grow inwards (fig 3–4).
If a patient presents with severe gingival recession, the speaker described a variation of the IDR protocol which should be used: the triple graft technique (da Rosa 2014). The ‘triple’ graft is a combination of connective tissue, cortical bone and particulate cancellous bone. It is harvested from the tuberosity using a scalpel and chisels. The graft is placed with the connective tissue layer facing the gingiva, and the cortical and cancellous bone facing the implant. A single suture in the middle is used to fix the graft in place, and two more sutures are used on each side in the papillae. A temporary crown is screwed with its margin levelled to the neighbouring teeth, without soft tissue recession, and leaving a gap for the tissue to grow in (fig 5–6). The speaker presented a case where this procedure was successfully used, with a 10-year follow-up. This technique can be applied even in cases where several bone walls have been lost, using autogenous block and particulate bone compacted through site preparation (da Rosa et al., 2019).
The final case presented by the speaker involved two central incisors which could not be maintained, with complete loss of the interdental papillae and partial loss of the lateral papillae. In this case an orthodontic approach was selected prior to surgery and extrusion was performed in order to gain bone and soft tissue vertically. After that, the incisors were extracted and the IDR technique was used.
Presentation figures
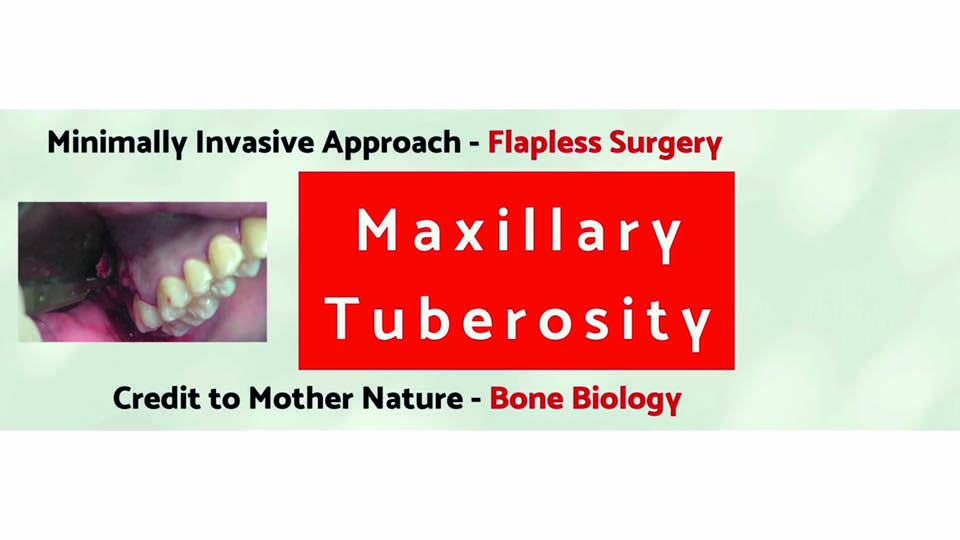
Fig 1: The technique donor site
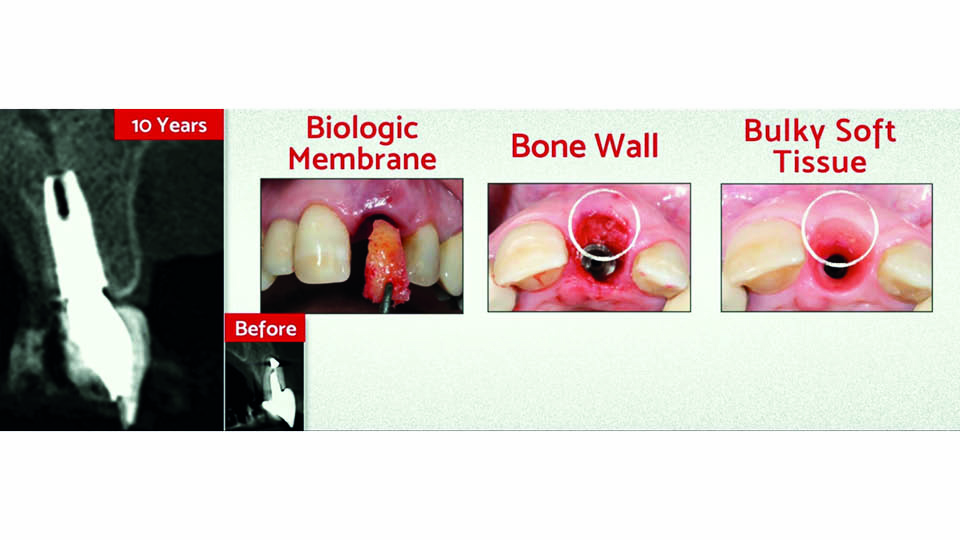
Fig 2: A biologic membrane of cortico-cancellous bone
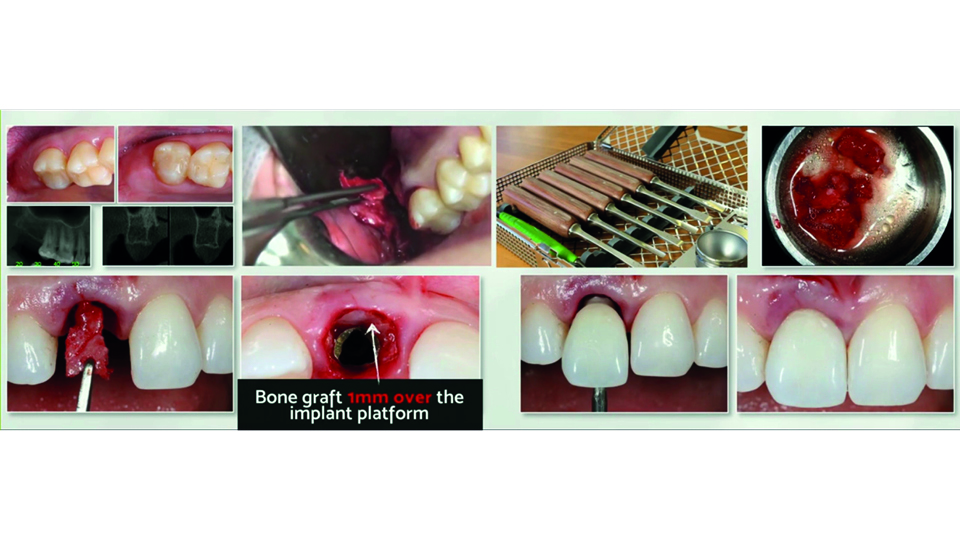
Fig 3: Harvesting the graft with chisels
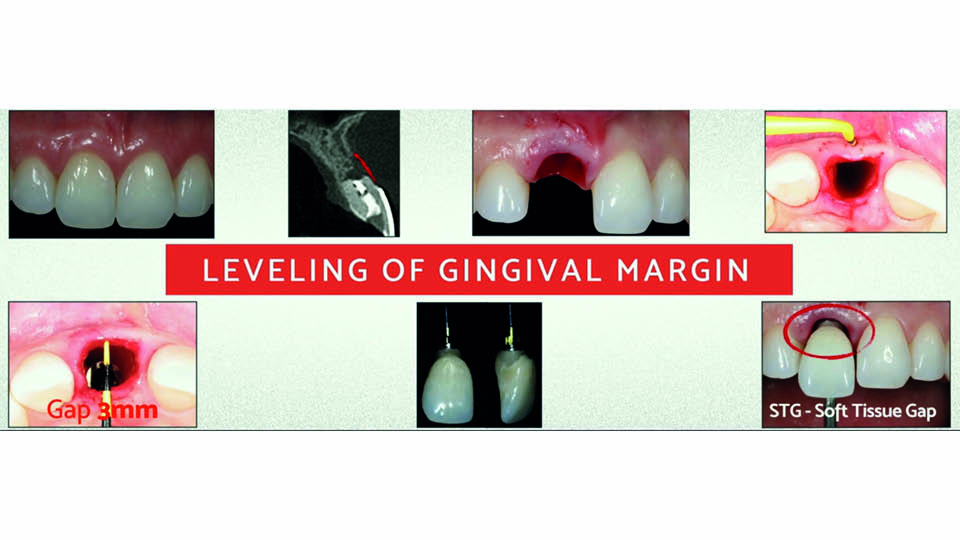
Fig 4
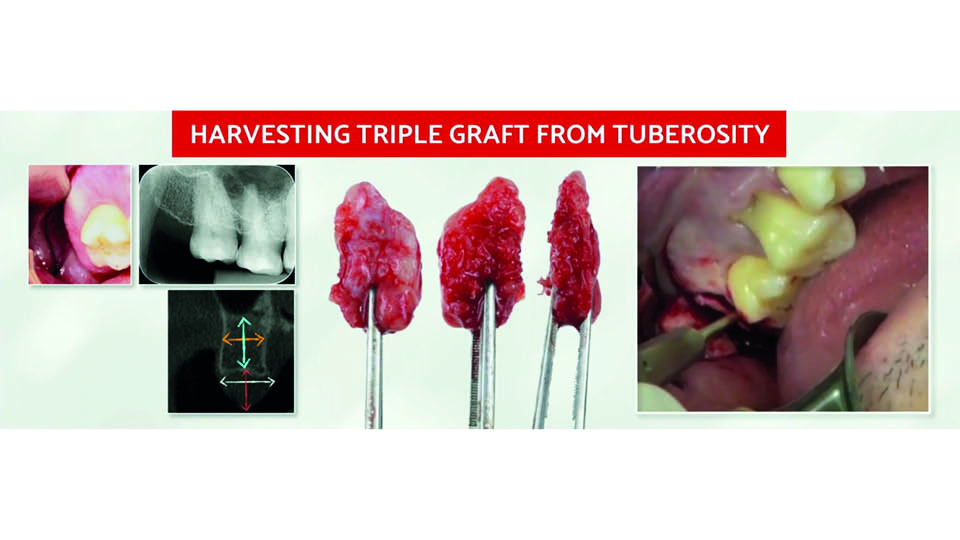
Fig 5
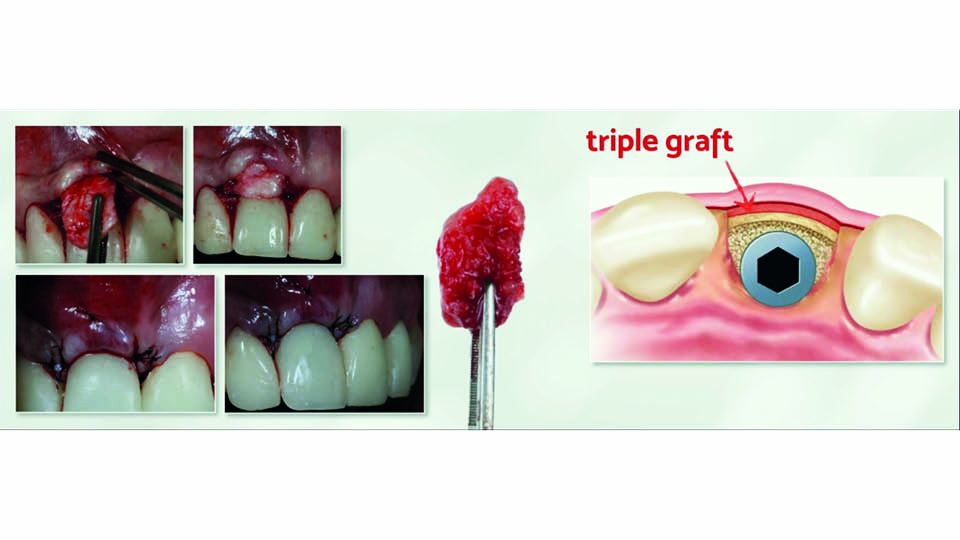
Fig 6
References:
da Rosa JC, Rosa AC, Fadanelli MA, Sotto-Maior BS. Immediate implant placement, reconstruction of compromised sockets, and repair of gingival recession with a triple graft from the maxillary tuberosity: a variation of the immediate dentoalveolar restoration technique. J Prosthet Dent. 2014;112(4):717-22.
da Rosa JCM, Pértile de Oliveira Rosa AC, Huwais S. Use of the Immediate Dentoalveolar Restoration Technique Combined with Osseodensification in Periodontally Compromised Extraction Sites. Int J Periodontics Restorative Dent 2019;39(4):527-34.
Rosa JC, Rosa AC, Francischone CE, Sotto-Maior BS. Esthetic outcomes and tissue stability of implant placement in compromised sockets following immediate dentoalveolar restoration: results of a prospective case series at 58 months follow-up. Int J Periodontics Restorative Dent 2014;34(2):199-208.
Rosa AC, da Rosa JC, Dias Pereira LA, Francischone CE, Sotto-Maior BS. Guidelines for Selecting the Implant Diameter During Immediate Implant Placement of a Fresh Extraction Socket: A Case Series. Int J Periodontics Restorative Dent 2016;6(3):401-7.
The L-PRF solution
The speaker recommended leucocyte-platelet rich fibrin (L-PRF) when treating defective sockets with buccal bone loss after tooth extraction. The L-PRF may be used in two protocols: ridge preservation or horizontal bone augmentation with L-PRF bone blocks (fig 7–8).
L-PRF preparation is subject to the following strict (but simple) protocol. Blood is centrifuged for 12 minutes in 8–16 tubes with silica coating, without any additives. If the patient is receiving anticoagulant treatment, their blood should be centrifuged longer. Once the tube is filled, centrifugation must begin no more than one minute after blood extraction, otherwise sub-optimal membranes will be formed. The centrifuge should be initially set up with two tubes; more tubes are then added, always two at a time in order to keep the centrifuge balanced.
Ridge preservation with L-PRF
The technique is performed with L-PRF alone, which acts as a scaffold. After extracting the tooth and removing the granulation tissue, at least three or four L-PRF membranes (or ‘plugs’) are inserted into the socket and condensed. The speaker then explained that the socket must be sealed by one or two more L-PRF membranes placed around the entrance to the socket in an envelope between the periosteum and the bone (by tunnelling the mucoperiosteum).
No post-surgical corticosteroids or antibiotics are needed, since the graft is 100% autogenous and rich in leucocytes. The speaker described some cases involving successful buccal bone plate regeneration three months after L-PRF ridge preservation.
The technique is well-documented, and it has been shown to result in lower levels of post-extraction alveolar bone resorption. Further, enhanced healing has also been shown after extraction of the third molar, with less reported pain, faster soft tissue healing and better bone quality (Temmerman et al., 2016; Castro et al., 2017a; Castro et al., 2017b).
Horizontal augmentation with L-PRF bone-block
In cases with major bony defects, the recommended approach is to use the L-PRF bone-block technique. For this, the graft should be a combination of L-PRF membranes divided into small pieces and mixed with bone substitute in a 1:1 ratio. Liquid fibrinogen, obtained with the same centrifugation method but with plastic coated tubes and three minutes of centrifugation, is added to this mixture to obtain a ‘strong’ block. The fibrin bone block obtained in this way will have appropriate mechanical qualities for bone regeneration. The block is covered with a collagen membrane which is further covered by L-PRF membranes; the latter of which is to improve the soft tissue healing above. Both membranes should be pinned to improve the stability of the graft (fig 9). This technique has been reported to achieve a mean horizontal ridge augmentation of 4.5mm, and a mean resorption rate during the healing phase of 16% (Cortellini et al., 2018).
Presentation figures
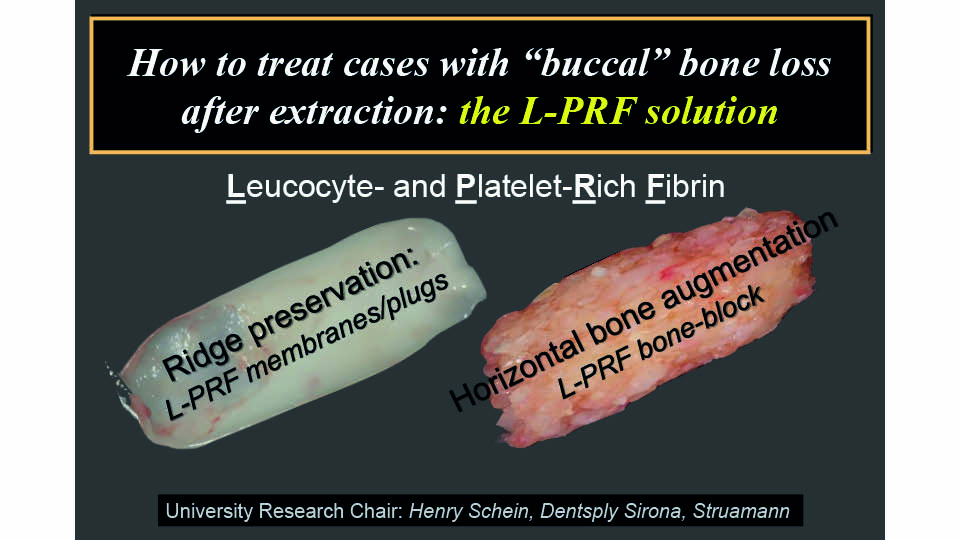
Fig 7
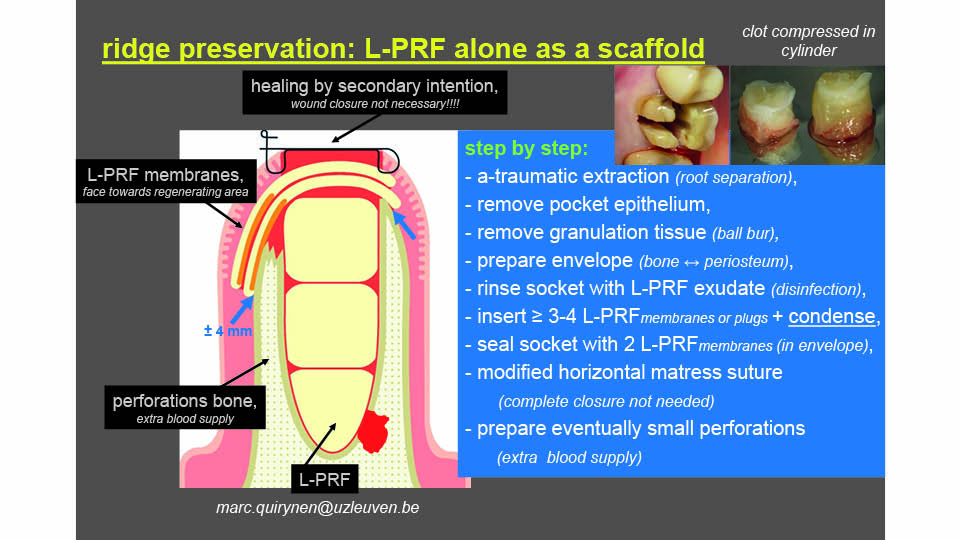
Fig 8
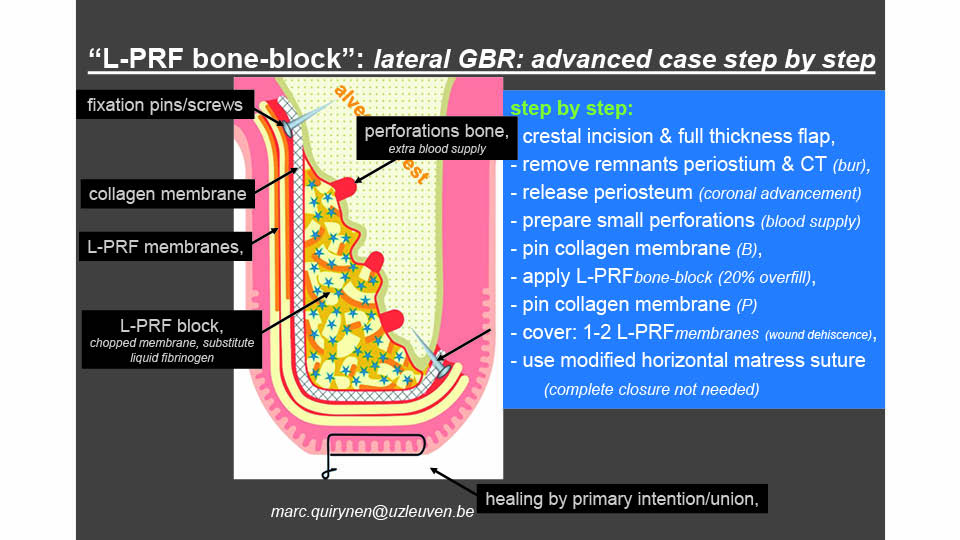
Fig 9
References:
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, Quirynen M. Regenerative potential of leucocyte- and platelet-rich fibrin. Part B: sinus floor elevation, alveolar ridge preservation and implant therapy. A systematic review. J Clin Periodontol. 2017 Feb;44(2):225-234. doi: 10.1111/jcpe.12658. Epub 2017 Jan 10. Review. PubMed PMID: 27891638; PubMed Central PMCID: PMC5347939.
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, Quirynen M. Regenerative potential of leucocyte- and platelet-rich fibrin. Part A: intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J Clin Periodontol. 2017 Jan;44(1):67-82. doi: 10.1111/jcpe.12643. Epub 2016 Nov 24. Review. PubMed PMID: 27783851; PubMed Central PMCID: PMC5248642.
Temmerman A, Vandessel J, Castro A, Jacobs R, Teughels W, Pinto N, Quirynen M. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: a split-mouth, randomized, controlled clinical trial. J Clin Periodontol. 2016 Nov;43(11):990-999. doi: 10.1111/jcpe.12612. Epub 2016 Sep 21. PubMed PMID: 27509214.
Cortellini S, Castro AB, Temmerman A, Van Dessel J, Pinto N, Jacobs R, Quirynen M. Leucocyte- and platelet-rich fibrin block for bone augmentation procedure: A proof-of-concept study. J Clin Periodontol. 2018 May;45(5):624-634. doi: 10.1111/jcpe.12877. Epub 2018 Apr 10. PubMed PMID: 29421855.
The soft tissue solution
There are several well-known techniques used to compensate for tissue changes following tooth extraction (Chappuis et al., 2017). Of these, the most commonly used is to rebuild the buccal part of the socket by bone grafting. Since the mid-90s, however, different soft tissue techniques have been proposed to build up the lost volume and seal the socket. A recent RCT compared CBCT images of guided bone regeneration (GBR) and soft tissue grafting, and concluded that both procedures were equally effective in the short term (De Bruyckere et al., 2018). On the other hand, however, a lower percentage of mineralisation has been observed in sockets where biomaterials are used (12%) compared with natural healing (50–60%) (Araujo et al., 2015).
The approach presented here by the speaker, for immediate implant placement in a defective socket with buccal bone wall loss, is based on a similar approach: let the socket heal naturally and protect it with a soft tissue graft. The implant should be placed palatally, allowing the blood clot to occupy the buccal space and form new bone. Next, a connective tissue graft is performed using a bilaminar tunnelling technique. This graft compensates for the loss of buccal volume and seals the socket (fig 10).
The speaker said he realises that this approach may be viewed as controversial, as it doesn’t pretend to fully recover the bone loss. But, he stated, we must accept that it can successfully maintain the total buccal volume of the socket, allowing us to opt for an immediate restoration.
Technically, the critical step in this technique is to create an adequate bilaminar bed for the soft tissue graft in a mean buccal mucosa thickness of 0.6mm. Part of the connective tissue graft is left exposed, to close the socket. The speaker showed several successful cases with 5–6 years of follow-up (which were progressively more difficult and complex); he also showed some recent cases with promising results (fig 11–12).
In cases involving extensive damage to the buccal bony wall, a second connective tissue graft may be needed. This technique – compensating alveolar socket seal (CASS) – has been used in 389 consecutive patients in the last ten years, on 414 implants, without biomaterials, with a 98.8% survival rate. Re-grafting with another CTG was needed in only 11 cases (data non published yet).
The speaker summarised the pros and cons of the CASS technique thus:
- Advantages: it maintains buccal volume and controls the height of buccal margin. There is no need for foreign material, thus promoting natural socket healing. It has reduced cost and associated chair time
- Disadvantages: it requires a second surgery site, specific microsurgical instruments and has a steep learning curve. It is a sensitive technique that should be classified as complex-advanced (Buser et al., 2017)
Presentation figures
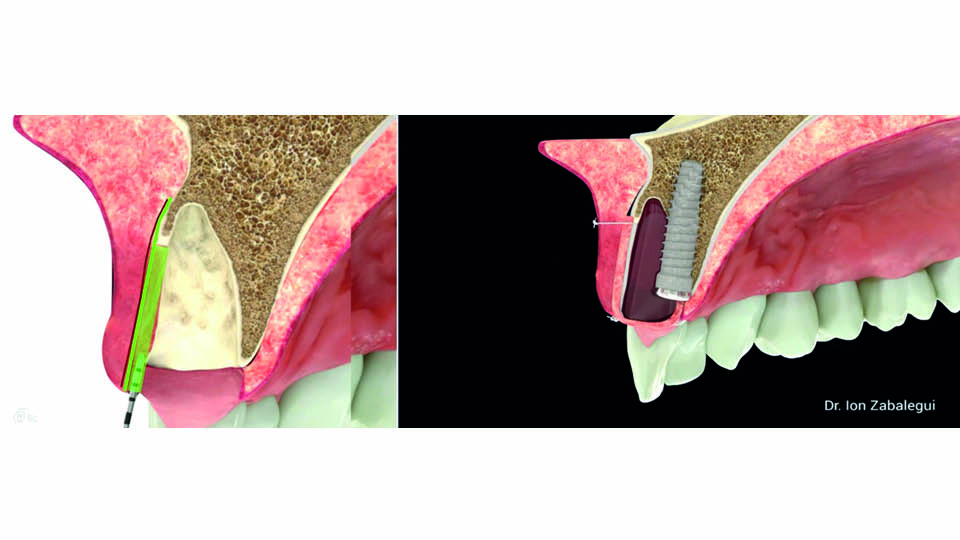
Fig 10: A CTG compensates the loss of volume

Fig 11: Clinical case

Fig 12: Long-term results
References:
Araújo MG, da Silva JCC, de Mendonça AF, Lindhe J. Ridge alterations following grafting of fresh extraction sockets in man. A randomized clinical trial. Clin Oral Implants Res 2015;26(4):407-12.
Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017 Feb;73(1):84-102.
Chappuis V, Araújo MG, Buser D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol 2000, 2017;73(1):73-83.
De Bruyckere T, Eeckhout C, Eghbali A, Younes F, Vandekerckhove P, Cleymaet R, Cosyn J. A randomized controlled study comparing guided bone regeneration with connective tissue graft to re-establish convexity at the buccal aspect of single implants: A one-year CBCT analysis. J Clin Periodontol 2018;45(11):1375-87.



