Revisiting implant controversies
Immediate placement and immediate loading: current and future outlook
Staged placement approach
As clinicians, our goal is to achieve perfect aesthetics and a high-scoring PES index (Fürhauser et al., 2005). To do this, extra soft tissue is required after rebuilding the hard and soft tissues. This is because the ideal soft tissue profile is achieved by pressure moulding it with the final suprastructure. To this end, the speaker recommended a one-piece crown with a convex transmucosal zone to push the tissue up during the prosthetic procedure.
Immediate implant placement is feasible, but… it should be performed with soft tissue augmentation and a staged approach. Otherwise, the extra soft tissue that is required will not be available in the prosthetic phase. The speaker said that we should let the soft tissue graft heal for four months before connecting the final suprastructure.
The current trend to use immediate implants/restorations in almost every case is adventurous
According to the speaker’s practice, about 10% of cases in the aesthetic area are treated using immediate implant placement (only those with no defects in the buccal bone or plate). 85% of cases do show buccal bone defects, and so are treated by early implant placement plus GBR. In the 5% of the remaining cases, neither perfect implant placement nor stabilisation of the membrane are possible, and so they are treated with a staged approach.
Biological limitations require a step-by-step approach
High probing values indicate that attachment is lost and bone is deficient. When extracting the involved teeth, additional high levels of remodelling will occur, meaning that immediate implants are not recommended. Further, if adjacent teeth must be extracted insufficient interproximal buccal bone will lead to loss of buccal papilla due to lack of support (Grunder et al., 2005). Buccal bone should be augmented first, and soft tissue volume increased next in a staged approach. This, the speaker said, is the only way to predictably ensure outcomes.
A non-resorbable and 3D-shaped membrane is needed for successful GBR
In most cases, the resorption time of the membrane greatly influences the outcome. The speaker outlined several cases with a minimum healing time of six months before membrane removal. Some native collagen membranes lasting less than two months may be useful for other applications. However, a very predictable way to pre-form the new bone as required is to use a titanium-reinforced PTFE-membrane. This is because it is non-resorbable and can be shaped in 3D. No biomaterials are required underneath.
The new bone formation (beyond the genetically determined skeletal envelope) has several requirements (fig 1):
- blood clot protection to prevent soft tissue from going into the space
- space maintaining, so volume is not lost as the space collapses
- stabilisation throughout the healing period
- time (especially when bone is to be created outside the skeletal envelope)
Flap design is key. The flap should be released in order to cover the augmented space in a tension-free way. This is a technique-sensitive procedure.
But it is not only bone that is needed: a subepithelial connective soft tissue graft is also needed (fig 2). In order to quickly harvest a uniform graft from the palate the speaker uses a mucotome (Mörmann et al., 1977) to de-epithelialised the area in the lateral palate as shown in Zuchelli’s well-known procedure before harvesting the subepithelial connective soft tissue.
Summary:
It’s all about case selection. When no buccal bone defects are present, immediate implant placement can be used in the aesthetic zone; however, the speaker said he always performs a simultaneous soft tissue graft and observes a four-month healing period before commencing the restoration procedure. When bone defects are present, the speaker prefers to: extract the tooth; wait two months for soft tissue healing; perform implant placement plus bone augmentation; wait six months and then perform the soft tissue graft; and then one month later start the second stage procedure. So, the total treatment time can last up to one year (fig 3).
The speaker emphasised the importance of timing for ideal aesthetics, and urged the audience to take their time.
Presentation figures

Fig 1: GBR requirements
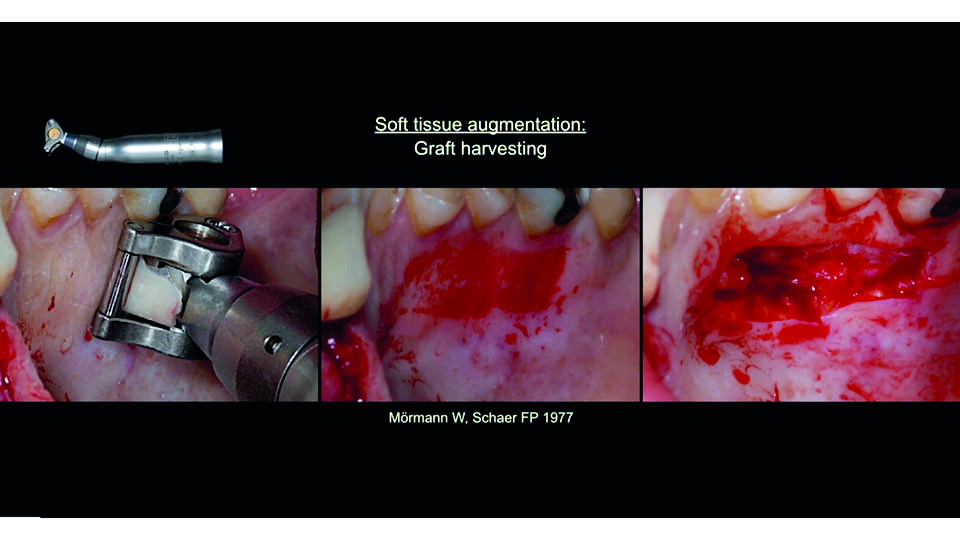
Fig 2: CTG harvested with mucotome
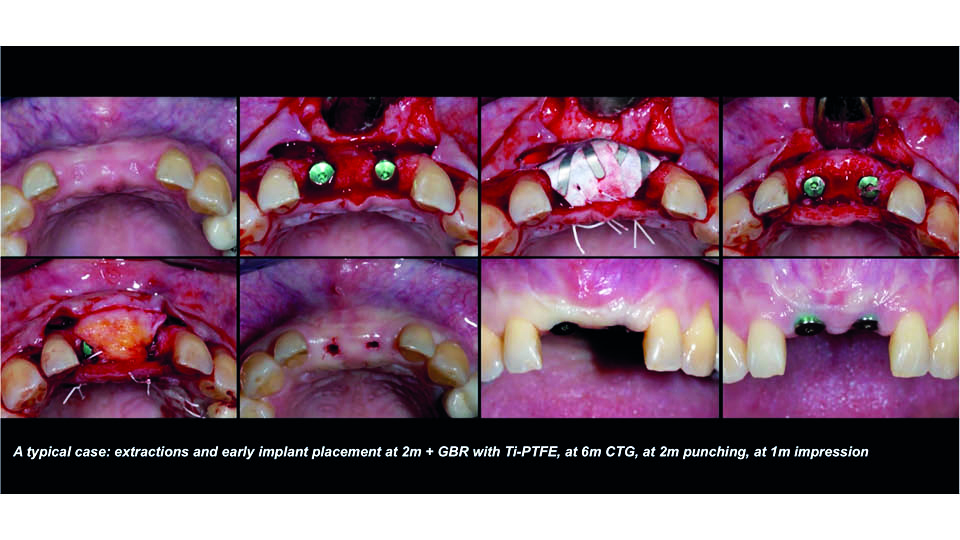
Fig 3: Sequence of a 2-year treatment
References:
Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-9.
Mörmann W, Schaer FP. [Transplantation of oral mucosa using a mucotome]. [Article in German]. SSO Schweiz Monatsschr Zahnheilkd. 1977;87(8):656-66.
Immediate placement approach
Immediate implant placement is controversial, since the clinical evidence we have is relatively low – population sizes are too small in the studies – and almost every conclusion is based only on case series. The speaker stated that they would not review the existing literature but would present his own experience and studies.
Looking for predictability: reducing technique sensitiveness
We all want predictability for our patient’s well-being, and we want to prevent failures. Immediate placement in the aesthetic zone is considered to be very technique-sensitive. It largely depends on the operator, which makes predictability difficult to achieve. But what we need are treatment procedures with universal reproducibility: treatments where people can rely on getting the same results across the board. This is what the speaker claims to have achieved with new implant and attachment designs.
The chamber concept: more space, better soft tissue formation
The speaker illustrated designs using the ‘chamber concept’ (Degidi et al., 2013). The ‘chamber’ is a three-dimensional biological space produced by combining:
- Sub-crestal implant placement
- Narrow-diameter abutments
A larger space is then left to be occupied by the blood clot, to allow the formation of new connective tissue (fig 4).
Then, the provisional is made using a special conometric coping retained by friction on the abutment. This removes the need for cementation (which could disturb this biological space).
Immediate implants with immediate loading in the aesthetic area: a protocol that works
The speaker then outlined the key factors for immediate placement with immediate loading in the aesthetic zone:
- Surgical procedures should be flapless, to maximise vascularisation in the buccal wall
- Primary stability must reach ≧ 25Ncm. To measure the implant stability, the speaker proposed a new parameter: variable torque work (VTW) (Degidi et al., 2013). VTW is the integral of the insertion torque curve during implant insertion. This measure seems to be more representative of the torque work required to insert an implant in the bone (as it represents the progressiveness of the curve). Further, square threads and a morse taper are important features for preventing implant micromotion (fig 5)
- Implants should be placed sub-crestally and anchored to the lingual cortical bone, far from the buccal wall and 2–3 mm deep (Degidi et al., 2011 /A)
- The vestibular gap should be filled by packing the graft particles in the middle and apical areas. The cervical space is part of the chamber and should not be filled
- Platform switching works, but must be used along with leaving the chamber space free for the connective tissue
- ‘One abutment, one time’ (Degidi et al., 2011 /B, 2014). The abutment should be placed simultaneously with the implant and not removed. Provisional and definitive prostheses are made over it. This concept is particularly effective with narrow abutments
- Immediate loading is beneficial when the implant is placed properly (Degidi et al., 2009)
- Gap-free restoration: the speaker’s conometric concept can be used, which avoids cement and screws. The protocol is based on conical copings with friction fit over the abutment
But there are limitations which should not be overlooked
The buccal bone wall should be intact. If it is partially lost, some cases may be possible to proceed with the protocol. But if it is completely lost, it would be unsafe to proceed.
Soft tissue should be favourable (or at least neutral). If there is insufficient soft tissue, the case will be more complicated and hence technique-sensitive. As a general rule: more complicated cases are more technique-sensitive, and so are less predictable.
Presentation figures
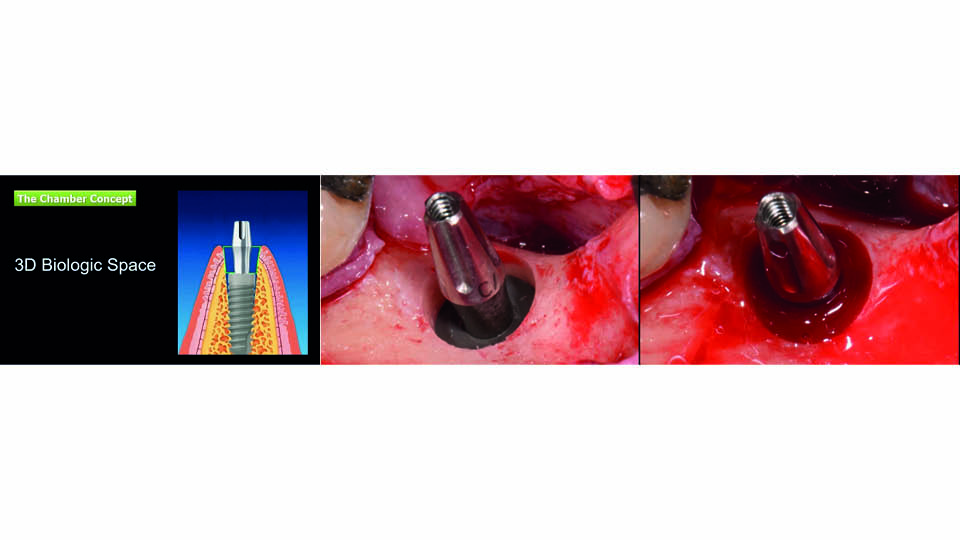
Fig 4: The “chamber concept”
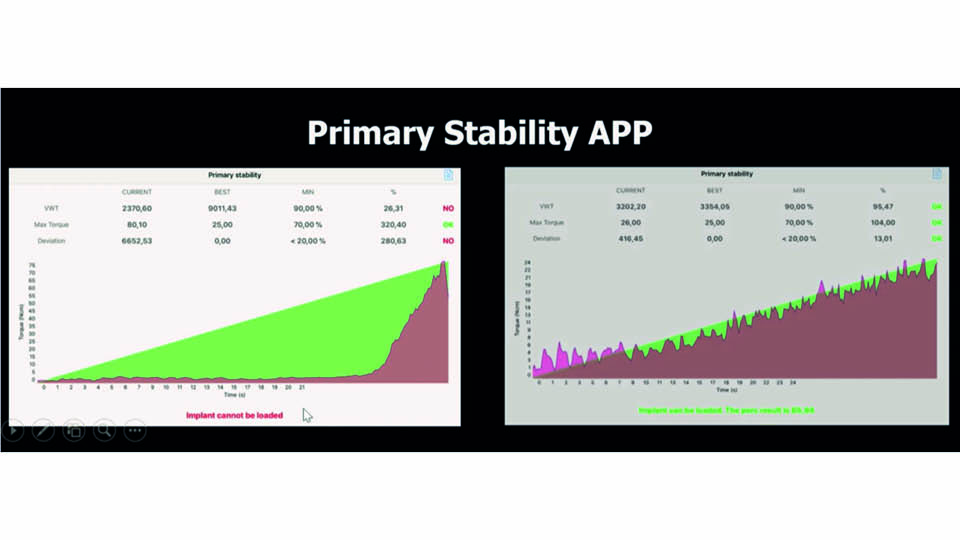
Fig 5: The “Variable Torque Work”
References:
Degidi M, Daprile G, Nardi D, Piattelli A. Immediate provisionalization of implants placed in fresh extraction sockets using a definitive abutment: the chamber concept. Int J Periodontics Restorative Dent 2013;33(5):559-65.
Degidi M, Daprile G, Piattelli A, Iezzi G. Development of a new implant primary stability parameter: Insertion torque revisited. Clin Implant Dent Relat Res. 2013;15(5):637-44.
Degidi M, Perrotti V, Shibli JA, Novaes AB, Piattelli A, Iezzi G. Equicrestal and subcrestal dental implants: a histologic and histomorphometric evaluation of nine retrieved human implants. J Periodontol 2011;82(5):708-15 /A.
Degidi M, Nardi D, Piattelli A. “One abutment at one time: non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants.” Clin Oral Impl Res, 2011;22:1303-7 /B.
Degidi M, Nardi D, Daprile G, Piattelli A. Nonremoval of immediate abutments in cases involving subcrestally placed post extractive tapered single implants: a randomized controlled clinical study. Clin Implant Dent Relat Res 2014;16(6):794-805.
Degidi M, Nardi D, Piattelli A. Immediate versus one-stage restoration of small-diameter implants for a single missing maxillary lateral incisor: a 3-year randomized clinical trial. J Periodontol 2009;80(9):1393-8.



