Revisiting implant controversies
When to save or “extract” an implant in the aesthetic zone
What are the indications and limitations of GBR
3D implant position in not negotiable
First, the speaker focused on hard and soft tissue deficiencies which are not associated with peri-implantitis. He stated that most of these problems arise from incorrect implant placement. For this reason, 3D implant positioning is crucial – he stated that if an implant cannot be placed in the exact 3D position, today is not the day to place it.
There is evidence in the literature supporting the fact that excessive buccal angulation is a strong predictor for mid-facial recession (Cosyn et al., 2012a). Placing implants in an alveolar process with missing buccal bone wall usually leads to apical displacement of the mucosal margin (Cosyn et al., 2012b) (fig 1).
GBR cannot correct peri-implant problems outside the bony envelope
The key factor for successful GBR is that it is applied within the contour of the bone. Outside the bony envelope, GBR is unpredictable; this is the limit for when GBR is indicated. When the implant platform is too close to the buccal bone wall, our therapeutic tools are not predictable enough. Finally, when implants are not placed deep enough in the bony envelope, regeneration is not predictable above the level of the implant-abutment connection (fig 2).
GBR can be used to augment deficiencies caused by peri-implantitis after tissues have healed. However, it is not indicated for correcting the effects of implants which have been placed too buccally.
In some cases, a connective tissue graft can improve both tissue sealing and aesthetic appearance by covering the greyish area. But the more buccally tilted the implant is, the less predictable the graft will be. Angulations over 25º are pointing outwards and should be explanted rather than treated.
Lack of keratinised tissue and recessions are limitations for GBR
There are thousands of implants which have been placed without buccal cortical bone. In these borderline situations, GBR results are unpredictable because of the lack of bone and keratinised tissue. If the implants don’t show signs of disease and can be well maintained by the patient, we should leave them as they are.
Prevention means placing the implant in the correct position
A systematic review has investigated the effect of various surgical and restorative interventions at immediate implant placement on the buccal mucosal level. Lingual-palatal implant positioning was found to be the intervention that most consistently prevented mid-buccal mucosal recession. Other interventions which had conflicting results were: platform-switching abutments, flapless approaches, gap grafting, connective tissue grafts and immediate provisionalisation (Lin et al., 2014).
Presentation figures
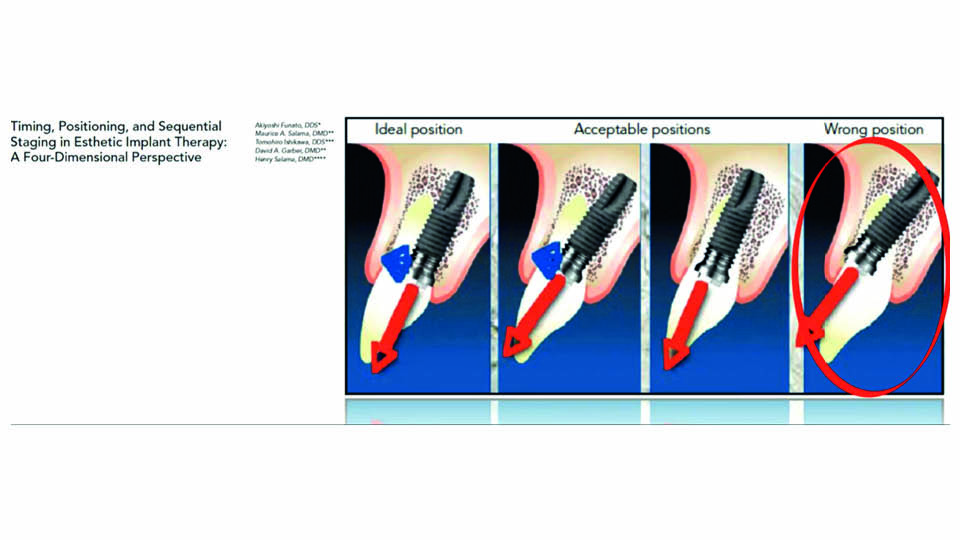
Fig 1: Implant position is not negotiable
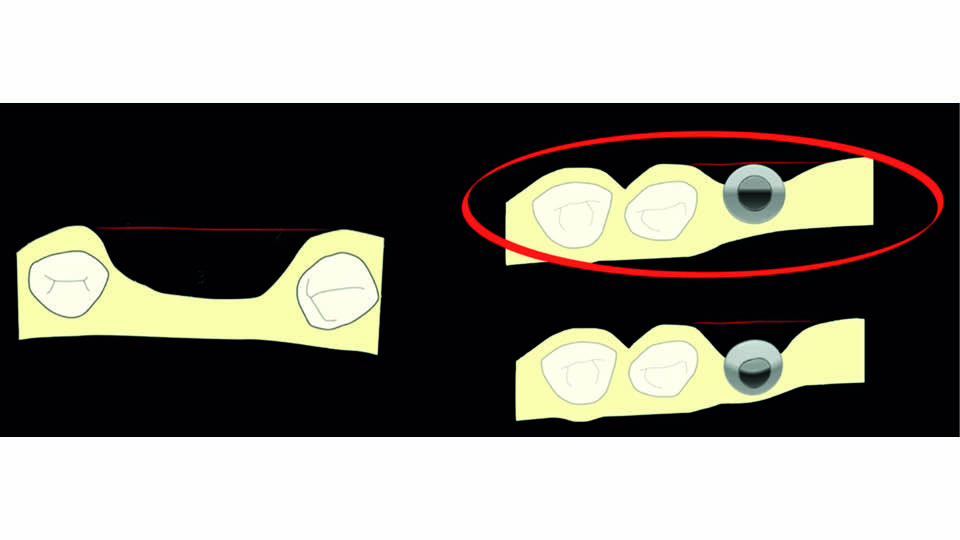
Fig 2: GBR not predictable out of the bony envelope
References:
Cosyn J, Sabzevar MM, De Bruyn H. Predictors of inter‐proximal and midfacial recession following single implant treatment in the anterior maxilla: a multivariate analysis. J Clin Periodontol 2012 A;39(9):895-903.
Cosyn J, Hooghe N, De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol, 2012 B;39(6):582-9.
Lin GH, Chan HL, Wang HL. Effects of currently available surgical and restorative interventions on reducing midfacial mucosal recession of immediately placed single‐tooth implants: a systematic review. J Periodontol, 2014;85(1):92-102.
When is it needed to remove an implant to solve an aesthetic problem
We still don’t know which technique for cleaning implants is best
Sometimes, inflammation can arise even in a correctly positioned implant, and we need to resolve this. The decision to explant is a difficult one to make, especially for the patient. The key factor is to properly decontaminate the implant surface; the problem, however, is that there is insufficient evidence on the best technique for doing this (Cha et al., 2019; Keim et al., 2019).
The speaker described a new electrolytic cleaning device which has promising initial results, but it is still in an experimental phase (Ratka et al., 2019) (fig 3).
When an implant is in the wrong place, there is often no way to manage it. Bone augmentation has its limits, and the implant is the ‘fix point’. If the implant has been placed too buccally, it is difficult to manage this since a new contour would have to be built in order to cover what is outside the anatomy (fig 4). We can opt to remove the implant, but this will lead to significant bone defects (fig 5).
Can we predictably correct post-explant defects? Complication rates reported in the literature range from around 12% in horizontal augmentations and up to 45% in vertical augmentations (Rocchietta et al., 2008; Jensen & Terheyden 2009). From this, we can conclude that augmentation techniques do not seem very predictable for a patient, especially considering the fact they have already suffered a problem with implants.
Biology set the rules, and we must follow them. The speaker described the four steps of intramembranous bone formation, which have been well established in the literature, from blood clot to provisional matrix, to woven bone to new mature bone (Cardaropoli et al., 2003). The key factors on which bone (instead of scar tissue) formation depend are: vascularity, inductive factors and mechanical factors.
The rules for increasing predictability in GBR
- Bone formation begins on the exposed defect surfaces and grows directionally towards the middle portion of the defect. Therefore, the more walls the defect has the more predictable regeneration will be (Schenk et al., 1994)
- The distance between walls is another important factor. The closer the walls are, the more predictable bone formation will be (Avila et al., 2010)
- Autogenous bone chips can act as centres for nucleating bone formation (Simion et al., 2015)
- Autogenous bone promotes higher levels of bone formation than other biomaterials (Schmitt et al., 2013)
- Predictability decreases when augmented volume is outside the bone contours; this is because of compressive forces that change the shape of the graft (Oppenheimer et al., 2008)
Conclusions
Correct 3D implant positioning is paramount. In cases involving poorly positioned implants, we often have to extract the implant.
Digitally planning your approach is one of the best ways to facilitate the procedure and prevent complications. Computer-guided bone harvesting can help us be sure that the bone volume needed is available in donor zones, like the ramus (De Stavola et al., 2015).
When reconstructing a defect, it is important not to go outside the bone contour. Khoury’s approach ensures good vascularity inside the graft due to the use of particulate autogenous chips and the fixing of two thin cortical bones to rebuild the lost bone profile.
After four months, implants can be placed using a computer-guided approach; GBR can be performed using membranes and biomaterials. Throughout the whole procedure, proper handling of soft tissues is very important to keep the reconstruction protected and covered while healing.
Presentation figures
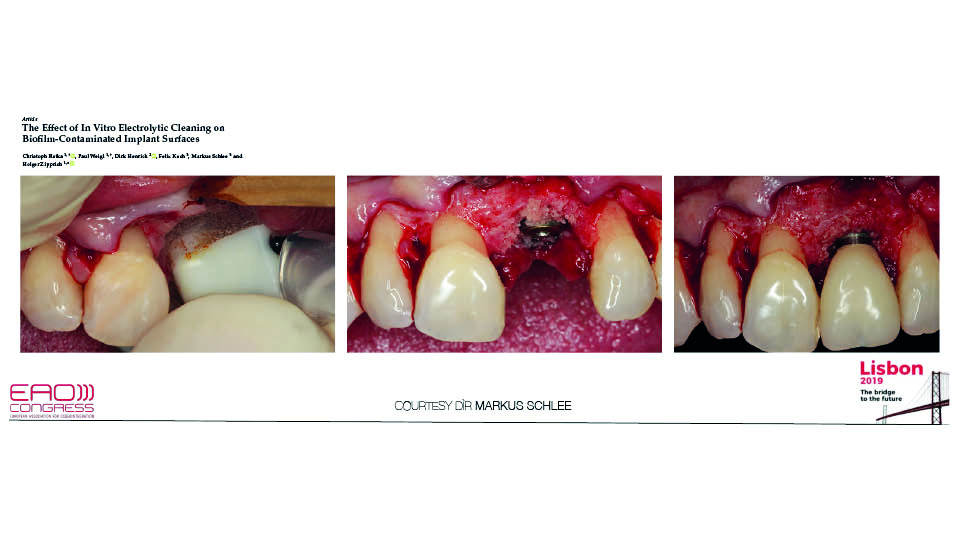
Fig 3: Surgical approach to decontaminate implant surface
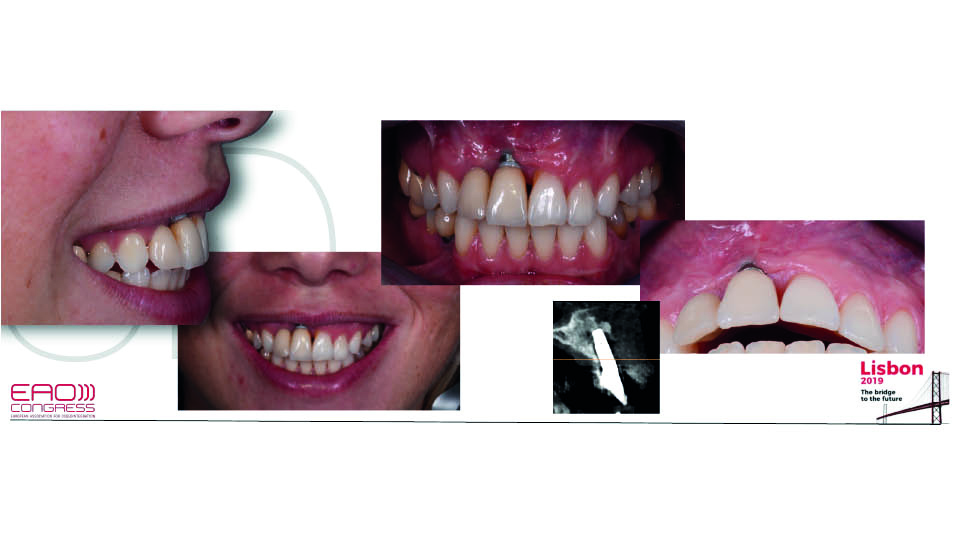
Fig 4: The implant has been placed too buccally
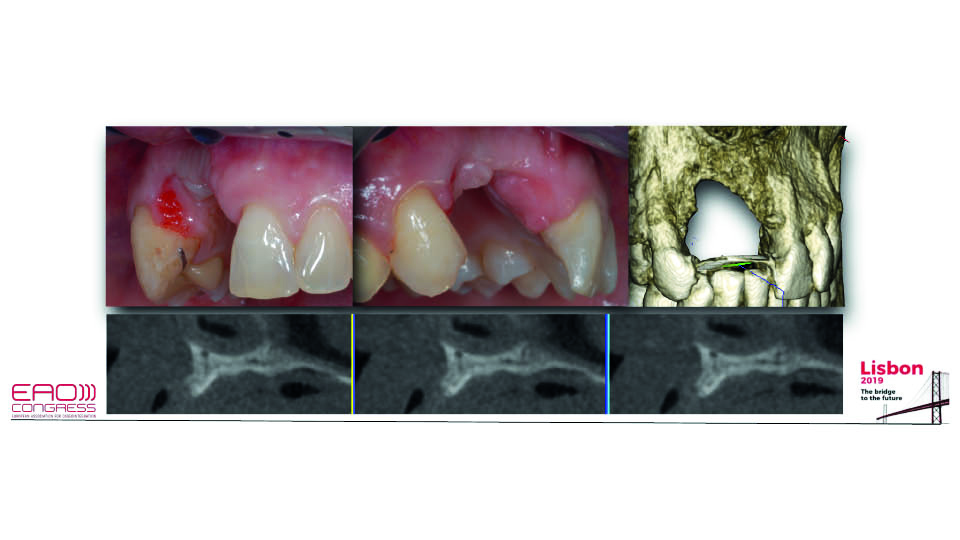
Fig 5: Defect post-explantation
References:
Avila G, Wang HL, Galindo-Moreno P, Misch CE et al. The influence of the bucco-palatal distance on sinus augmentation outcomes. J Periodontol. 2010;81(7):1041-50.
Cardaropoli G, Araújo M, Lindhe J. Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 2003;30(9):809-18.
Cha JK, Paeng K, Jung UW, Choi SH, Sanz M, Sanz‐Martín I. The effect of five mechanical instrumentation protocols on implant surface topography and roughness: A scanning electron microscope and confocal laser scanning microscope analysis. Clin Oral Implants Res, 2019;30(6):578-87.
De Stavola L, Fincato A, Albiero AM. A computer-guided bone block harvesting procedure: a proof-of-principle case report and technical notes. Int J Oral Maxillofac Implants. 2015;30(6):1409-13.
Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009;24Suppl:218-36.
Keim D, Nickles K, Dannewitz B, Ratka C, Eickholz P, Petsos H. In vitro efficacy of three different implant surface decontamination methods in three different defect configurations. Clin Oral Implants Res, 2019;30(6):550-8.
Oppenheimer AJ, Tong L, Buchman SR. Craniofacial Bone Grafting: Wolff’s Law Revisited. Craniomaxillofac Trauma Reconstr. 2008;1(1):49-61.
Ratka C, Weigl P, Henrich D, Koch F, Schlee M, Zipprich H. The Effect of In Vitro Electrolytic Cleaning on Biofilm-Contaminated Implant Surfaces. J Clin Med, 2019;8(9):1397.
Rocchietta I,Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. J Clin Periodontol. 2008;35(8 Suppl):203-15.
Schenk RK, Buser D, Hardwick WR, Dahlin C. Healing pattern of bone regeneration in membrane-protected defects: a histologic study in the canine mandible. Int J Oral Maxillofac Implants. 1994;9(1):13-29.
Schmitt CM, Doering H, Schmidt T, Lutz R, Neukam FW, Schlegel KA. Histological results after maxillary sinus augmentation with Straumann® BoneCeramic, Bio-Oss®, Puros®, and autologous bone. A randomized controlled clinical trial. Clin Oral Implants Res. 2013;24(5):576-85.
Simion M, Benigni M, Al-Hezaimi K, Kim DM. Early bone formation adjacent to oxidized and machined implant surfaces: a histologic study. Int J Periodontics Restorative Dent. 2015;35(1):9-17.
Aesthetic Complications, the Soft Tissue Approach
Soft tissue complications around implants are more difficult than around teeth
For teeth, we have well established classifications, prognostic tools and treatment strategies supported by scientific evidence. For peri-implant soft-tissue recessions, however, these are not so well established. The differences between teeth and peri-implant mucosa and gingiva may lead to impaired treatment results. But extracting implants has psychological concerns for the patient, especially in the aesthetic area. Hence, we need to treat them.
Several factors, most of which are out of our control, have recently been found to have prognostic value for covering peri-implant soft tissue deficiencies (Decker et al., 2017). These factors may come from:
- patient-related factors: systemic conditions, diabetes, smoking, oral hygiene habits
- local conditions: inflammation, interproximal bone/soft tissue, implant buccal/lingual position, tissue thickness and keratinised tissue width
The prognostic factors should be assessed before treatment
The speaker shared several diverse clinical cases where the above patient-related and local factors were assessed as part of a check-list before treating the peri-implant soft-tissue defects (Decker et al., 2017).
First of all, they assessed whether the causal factor could be removed. Then, the general health and habits of the patient were evaluated. Turning next to the local conditions, they checked if there were any signs of inflammation, interproximal bone loss, the bucco-lingual position of the implant and the soft tissue dimensions.
It has been shown that a prosthetic-surgical approach (switching to a narrower abutment for a short length of time and then grafting with connective tissue) can achieve good clinical results (Zucchelli et al., 2018). However, it seems that case selection is crucial for treatment success. Nevertheless, the soft tissue approach should be always tried first, since it is often the case that the only alternative is to remove the implant. Soft tissue correction is also the first choice because it is the least invasive approach.
Nowadays, implant dentistry is focused on achieving optimal aesthetic outcomes and long‐term clinical stability. New techniques for managing soft tissue are available and could be the key to meet the increasing aesthetic demands from patients. Soft tissue augmentation around implants is a unique tool for ensuring long‐term functional and aesthetic stability.
References:
Chackartchi T, Romanos GE, Sculean A. Soft tissue‐related complications and management around dental implants. Periodontology 2000, 2019;81(1):124-38.
Decker AM, Suárez-López Del Amo F, Urban IA, Miller PD Jr, Wang HL. Prognostic Classification System for Implant Recession Defects. Implant Dent. 2017;26(6):848-52.
Zucchelli G, Felice P, Mazzotti C, et al. 5-year outcomes after coverage of soft tissue dehiscence around single implants: a prospective cohort study. Eur J Oral Implantol. 2018;11:215-24.



