Dealing with complications
A growing problem: recessions around implants
How to prevent recessions around implants
Treatment goals should be viewed in the long-term
Our main treatment goal should be long-term aesthetic and functional success. This is closely associated with peri-implant stability of hard and soft tissues. Therefore, as well as having osseointegration as our basic objective, soft tissue integration is another pre-requisite for implant stability.
The supracrestal soft tissue – the so-called ‘biological width’ – may change with peri-implant bone remodelling.
Tissue structure around teeth and implants is different
Peri-implant tissue structure is the underlying cause for the high rate of recessions around implants. The connective tissue around an implant is more like scar tissue, with fewer fibroblasts and more collagen fibres than normal tissue. These collagen fibres are oriented parallel to the implant surface. Vascularisation of peri-implant tissues is lower than that of the periodontium. Hence, the healing and regenerative capacity of soft tissue around implants is lower than that of natural teeth; the occurrence and treatment of recessions should therefore be considered with this difference in mind.
But the main cause of recessions around implants is the dentist, as they can be at fault in the following ways:
- incorrect implant placement (too buccal)
- inadequate treatment of vestibular bone deficiencies
- discrepancy between size of implant and bony envelope
- inappropriate distance between implant(s) and teeth
- thin mucosa
- mucositis and/or peri-implantitis
The thickness of the mucosa translates to peri-implant bone loss
A mucosa thickness of 2mm is considered the parameter for predicting peri-implant bone loss. It has been shown that after one year, significantly more bone was lost in thin phenotypes (< 2mm) than thicker types (Puisys et al., 2015). Therefore, to augment mucosal thickness in cases involving thin phenotypes, reinforcing the biological seal and facilitating plaque control is recommended. The speaker uses a modified coronally advanced tunnel technique combined with a connective tissue graft to rebuild the contour of thin-tissue recessions. This surgical approach should be combined with the appropriate prosthetic procedure (Jurczyck et al., 2017) (figs 1–4).
A recent systematic review concluded that, despite the limited evidence, a lack of attached keratinised mucosa around implants makes them more prone to plaque accumulation, inflammation and recessions (Iorio-Siciliano et al., 2020).
To prevent recessions, we should consider whether the following are present:
- correct 3D implant positioning
- sufficient vestibular bone
- appropriate implant diameter in relation to the bony envelope
- adequate distance between implant(s) and teeth
- sufficient levels of attached mucosa and mucosal thickness
- infection control to prevent mucositis/peri-implantitis
Presentation figures
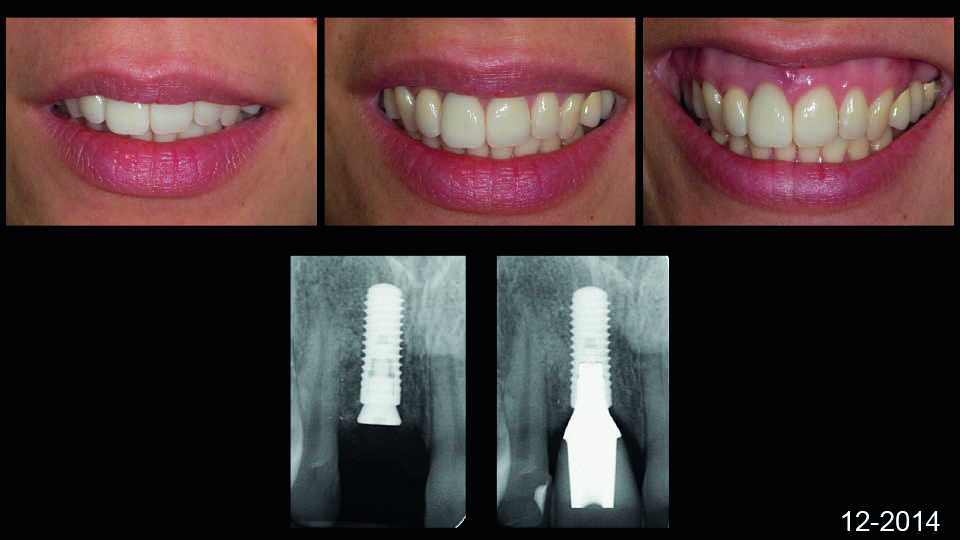
Fig 1: Treating peri-implant recession. A standard case

Fig 2: Treating peri-implant recession. A standard case

Fig 3: Treating peri-implant recession. A standard case

Fig 4: Treating peri-implant recession. A standard case
References:
Iorio-Siciliano V, Blasi A, Sammartino G, Salvi GE, Sculean A. Soft tissue stability related to mucosal recession at dental implants: a systematic review. Quintessence Int. 2020;51(1):28-36.
Jurczyck K, Belser UC, Sculean A. The management of peri-implant mucosa deficiencies in esthetic sites: case report of a combined surgical-prosthetic approach. Int J Periodontics Restorative Dent, 2017;37(6):808-17.
Puisys A, Linkevicius T. The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin Oral Implants Res, 2015;26(2):123-9.
Treatment of recessions around implants with the tunnel technique
From a clinical perspective, there is a difference between the risk factors associated with soft tissue dehiscence around implants and aetiological factors that can cause gingival recession.
Avoiding recessions: knowing the risk factors
The risk factors for tissue dehiscence around implants have been well documented (fig 5):
- thin phenotype
- lack of keratinised mucosa
- implant positioning
- thin (or lack of) buccal bone
The modified coronal advanced tunnel (MCAT) technique
The MCAT technique was first described to treat multiple gingival recessions (Aroca et al., 2010; ibid, 2013). However, it can also be performed for implant recessions.
The technique uses a full-thickness tunnelised flap, and is performed without a blade in order to keep the periosteum intact. The flap should be extended beyond the mucogingival line, where collagen and muscular fibres should be cut to free the flap from attachments. The implant surface is then thoroughly cleaned and a connective tissue graft is harvested from the palate and placed under the tunnelised flap. Finally, sliding sutures are placed to coronally mobilise the flap and completely cover the graft.
The distance between the tip of papilla to the contact point
The MCAT technique has been shown to give predictable results in multiple type III gingival recessions. The distance between the tip of the papilla to the contact point at the baseline is used as a prognostic parameter to show the root coverage achievable by the MCAT. When the distance measures ≦ 3mm in the maxilla, the probability of full coverage is 89%; in the mandible it is only 34% (Aroca et al., 2018).
MCAT and implant recessions
The speaker presented some complex cases which were successfully treated with the MCAT technique. In one case, the patient rejected the autogenous soft tissue graft and so the speaker opted to use MCAT plus collagen matrix to increase soft tissue levels six months before extraction. The tooth was then extracted and socket preservation was performed. After another six months the site was ready for implant placement, and, as the patient became more confident, a simultaneous connective tissue graft could be performed. One year after everything was stabilised, the definitive prosthesis was done.
The message is to prevent recession around implants
Proper soft tissue management before and at the time of implant placement is key. If tissue thickness is less than 2mm, soft tissue augmentation is recommended. Proper bone augmentation is also needed before and at the time of implant placement. In the absence of sufficient buccal bone wall (or if defects are present), bone augmentation is highly recommended.
Presentation figures
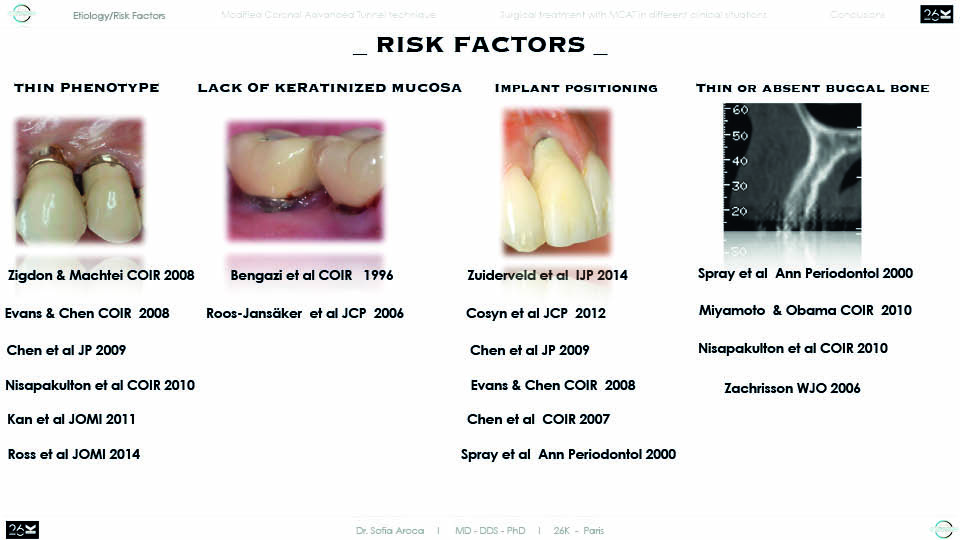
Fig 5: Risk factors of peri-implant recessions
References:
Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, Etienne D. Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol, 2010;37(1):88-97.
Aroca S, Molnár B, Windisch P, Gera I, Salvi GE, Nikolidakis D, Sculean A. Treatment of multiple adjacent Miller class I and II gingival recessions with a Modified Coronally Advanced Tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol. 2013;40(7):713-20.
Aroca S, Barbieri A, Clementini M, Renouard F, de Sanctis M. Treatment of class III multiple gingival recessions: Prognostic factors for achieving a complete root coverage. J Clin Periodontol. 2018;45(7):861-8.
Treatment of recessions around implants with the VISTA technique
Recessions around implants are a common problem. A systematic review revealed that 11% of immediately placed implants develop buccal mucosal dehiscence (Khzam et al., 2015). Another study focused on conventionally placed implants and found that the incidence of mucosal recession over 1mm was 61% (Oates et al., 2002). It can therefore be concluded that this is a frequent complication.
Recessions around implants pose severe aesthetic complications. Recessions have a considerable negative impact on the aesthetic result, as the patient considers it completely unacceptable and the problem requires further treatment (Cosyn et al., 2012; Sculean et al., 2017).
Treatment methods for root coverage around teeth have evolved over the years. They have become increasing predictable and currently employ a combination of tunnel access or coronally advanced flaps together with connective tissue grafts or soft tissue substitutes (Cortellini et al., 2012). Around implants, however, it is not yet clear which technique is the ‘gold standard’ (fig 6–7).
The evidence found in the literature is still limited and the results reported are variable. So far, the use of a coronally advanced flap combined with a connective tissue graft is considered the best option, with a success rate of around 90%. But these results should be taken with caution as they may be due to the operator’s skill and may depend on rigorous case selection (i.e. only single, healthy implants with adjacent teeth without interproximal attachment loss).
VISTA: a remote surgical access technique
The vestibular incision subperiosteal tunnel access (VISTA) technique was first described in 2011 (Zadeh et al., 2011). Unlike conventional tunnelling approaches, which use only a small intrasulcular incision, VISTA adopts an approach from a remote surgical access in the vestibule. A vertical incision is made in the vestibule, followed by the elevation of a subperiosteal tunnel towards the gingival margin. The tunnel releases the tension of the flap so a graft can be placed inside. The dissected tunnel is then coronally repositioned by horizontal mattress sutures bonded to the buccal surface of the teeth that anchor such coronal advancement and maintain it during the healing period (fig 8).
It has been shown that predictable root coverage and gingival volume gain can be achieved by the VISTA procedure; these results have been digitally measured and recently published (Gil et al., 2018; Gil et al., 2019). Results have also shown that initial root prominence is associated with less root coverage.
Case selection is crucial for good results. Risk factors for implant margin recessions have been well documented. There are anatomical factors (buccal position, thin biotype, lack of keratinised mucosa), pathological (peri-implantitis) and behavioural factors (smoking) which have been documented (Mazzoti et al., 2018).
Removing the implant may be the only solution in unfavourable cases
Some cases should not be selected for treatment. This is because recessions are highly dependent on underlying risk factors (i.e. implants positioned too buccally, narrow inter-implant distance or peri-implantitis).
When indicated (the implant is healthy, the placement is in the right position and the bone anatomy around the implant is favourable), however, VISTA can be an appropriate approach for treating implant recessions, due to its:
- remote surgical access, which does not disturb the delicate scar-like mucosal margin around an implant
- capacity to increase mucosal thickness in a predictable way with a connective tissue graft (placed properly on a secure bed) or a soft tissue substitute
- coronal flap displacement, which can be achieved by anchored sutures
Conclusions
- understanding the aetiology of the defect is key in case selection and treatment choice
- the evidence supporting surgical treatment is limited
- VISTA is a predictable technique for treating multiple recessions on teeth
- VISTA can also be used to manage implant recessions, although an RCT is needed to validate it
Presentation figures
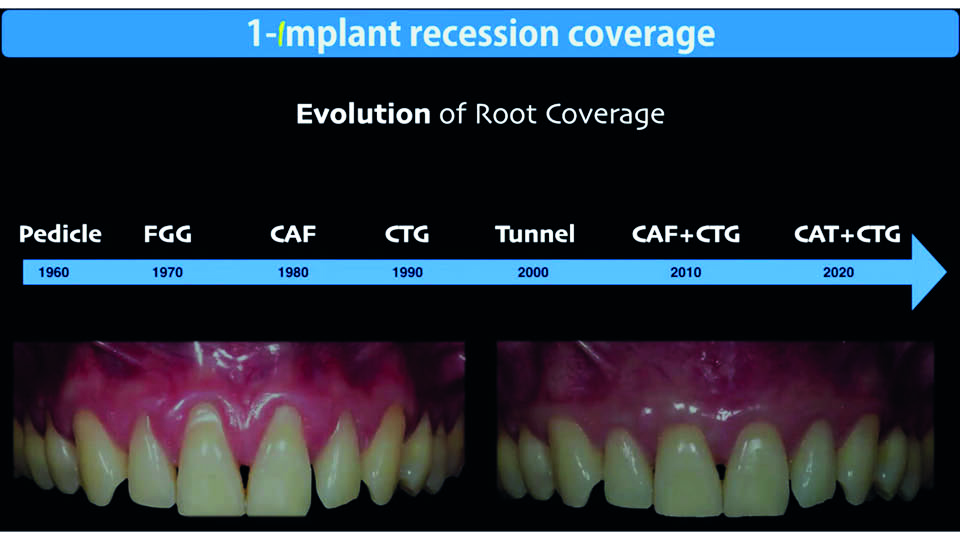
Fig 6: Root coverage. Evolution of treatments
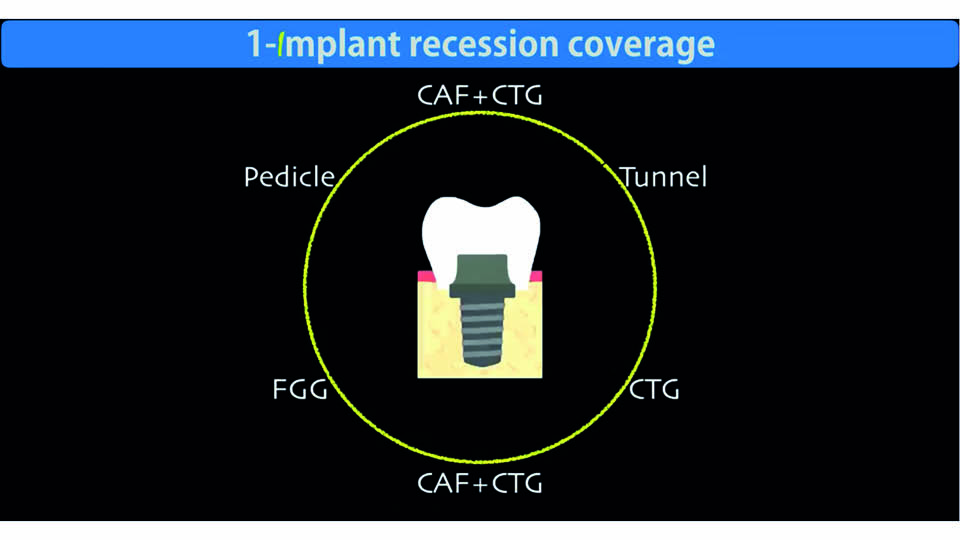
Fig 7: Peri-implant recession. Treatment options
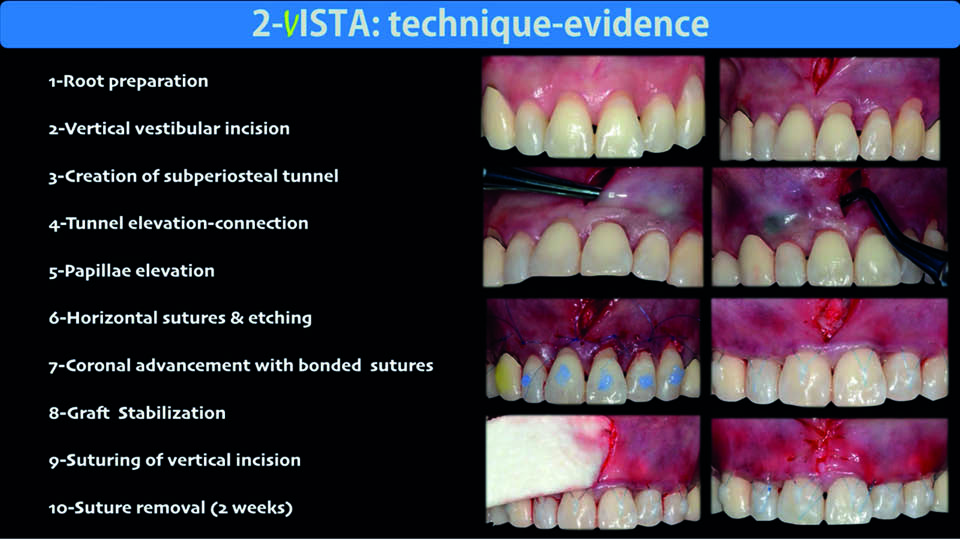
Fig 8
References:
Cortellini P, Pini Prato G. Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience. Periodontol 2000. 2012 Jun;59(1):158-84.
Cosyn J, Hooghe N, De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol. 2012;39(6):582-9.
Gil A, Bakhshalian N, Min S, Zadeh HH. Treatment of multiple recession defects with vestibular incision subperiosteal tunnel access (VISTA): A retrospective pilot study utilizing digital analysis. J Esthet Restor Dent. 2018;30(6):572-9.
Gil A, Bakhshalian N, Min S, Nart J, Zadeh HH. Three-Dimensional Volumetric Analysis of Multiple Gingival Recession Defects Treated by the Vestibular Incision Subperiosteal Tunnel Access (VISTA) Procedure. Int J Periodontics Restorative Dent. 2019;39(5):687-95.
Khzam N, Arora H, Kim P, Fisher A, Mattheos N, Ivanovski S. Systematic Review of Soft Tissue Alterations and Esthetic Outcomes Following Immediate Implant Placement and Restoration of Single Implants in the Anterior Maxilla. J Periodontol. 2015;86(12):1321-30.
Mazzotti C, Stefanini M, Felice P, Bentivogli V, Mounssif I, Zucchelli G. Soft-tissue dehiscence coverage at peri-implant sites. Periodontol 2000. 2018;77(1):256-72.
Oates TW1, West J, Jones J, Kaiser D, Cochran DL. Long-term changes in soft tissue height on the facial surface of dental implants. Implant Dent. 2002;11(3):272-9.
Sculean A, Chappuis V, Cosgarea R. Coverage of mucosal recessions at dental implants. Periodontol 2000. 2017;73(1):134-40.
Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent. 2011;31(6):653-60.



