New perspectives
Zirco-mania: where are we today and where are we heading?
Zirconia on teeth
The introduction of zirconia (ZrO2) was a milestone in the rapidly growing field of ceramics. The speaker started using zirconia fixed dental prostheses (FDPs) more than 20 years ago, when material was still relatively unknown, and was often mishandled. Infra-designed frameworks not supporting the veneer material often led to ceramic chipping, especially in long-span bridges. In a retrospective study on zirconia, the 10-year survival rate was 95.0% (CI 86–100%); however only 78.8% (CI 62.2–99.7%) were chip-free (Teichmann et al., 2018).
Another step forward was when open-pore pre-sintered zirconia became available for fabricating monolithic zirconia constructions.[1] This zirconia could be dry ground by carbide burs and the sinterisation was shorter, making the total process easier and quicker than before. Monolithic zirconia constructions were initially not particularly aesthetically pleasing, but the new frameworks occupied nearly all of the restoration’s profile, leaving only the minimum space needed to be veneered. This significantly reduced the amount of chipping, but did not totally eliminate it unless monolithic zirconia without veneering were used.
Indeed, the speaker highlighted that mechanical problems persist in veneered zirconia restorations, as shown in a 10-year RCT comparing fixed metal-ceramic prostheses with fixed zirconia prostheses. The study reported similar survival rates, but zirconia bridges were associated with significantly higher rates of framework fracture, de-bonding, major fractures of veneering ceramic and poor marginal adaptation (Sailer et al., 2018).
In an attempt to address these mechanical problems, the speaker described how their group had tried to strengthen the veneering material by replacing it with a CAD-CAM lithium disilicate glass-ceramic superstructure which fit perfectly on a specific designed zirconia framework. Both parts were fused together by sintering ceramic. At a mean follow-up of 13.9 months, this three-part ceramic restoration mostly exhibited just minor chipping compared with manually layered, zirconia veneered ceramic restorations (Grohmann et al., 2015).
Resin-bonded fixed dental prostheses (RBFDPs) are another application of zirconia. The speaker described an ongoing ten-year split-mouth study they are pioneering, comparing two wings of RBFDPs made of non-precious metal with zirconia in the restoration of upper missing laterals. Although the study has not been published yet, the most frequently encountered complication is the fracture between the pontic and the canine wing (Edelhoff et al., 2019B). It is now well known that cantilevered RBFDPs have fewer clinical failures in the anterior region (Wei et al., 2016). Some guidelines are recommended for the preparation of the abutment tooth, such as a slight chamfer finish, a 0.5mm-deep flat box in the connector side and a fossa in the centre (Edelhoff et al., 2019A). The ten-year survival rate of RBFDPs reached 98%, but the success rate is slightly lower, at 92%, due to some cases of de-bonding (Kern et al., 2017).
Adhesion
Proper adhesion of zirconia is a major factor for long-term clinical success. A recent systematic review concluded that physicochemical conditioning of zirconia leads to increased adhesion, and MDP-based[2] resin cements tend to offer better results (Özcan & Bernasconi, 2015). These results align with the protocol recommended by the International Academy for Adhesive Dentistry (Inokoshi & van Meerbeek, 2014).
Polishing
The outer surface should be manually polished. To achieve a smooth surface, a sequential application of all polishing steps should be followed (Preis et al., 2015). Regarding the matter of antagonist enamel wear that polished zirconia produces, in vitro studies show that this can be considered similar to that of natural teeth and less than that of metal-ceramics (Gou 2019). However, a higher number of clinical trials will be necessary to create a better assessment.
Four generations
ZrO2 has undergone several changes and continuous development over different generations, in attempts to achieve better light transmission to improve its aesthetic appearance. By the increase of light transmission for FDPs, it has lost strength (Zhang & Lawn, 2018; Kwon et al., 2018); this is why connector sizes should be increased (fig 3). The monolithic translucent zirconia of two generations (e.g. LavaTM Plus) offers an acceptable compromise between aesthetic appearance and strength (fig 4). Gradient technology (e.g. IPS e.max ZirCAD Prime) combines the translucency of 5Y-TZP with the strength of the 3Y-TZP. It should be noted that as there are different methods for measuring its mechanical properties, the information presented through advertising and marketing can be misleading.
Another interesting aspect of new monolithic zirconia is that it is less invasive. Indeed, it requires less tooth substance to be removed than any other all-ceramic crown, according to an in vitro comparative investigation (Schwindling et al., 2019).
Future perspectives
The speaker predicted that new developments in intraoral scanning will soon allow practitioners to look inside the tooth structure, to capture the internal morphology of the dentin core. This information can be built into the zirconia restoration to improve aesthetics. Furthermore, in the future the additive approach may be conducted via 3D printing (LaserCusing Process and 3D Binder Jetting).
Conclusions
- Zirconia is now not just one material, but a family of materials. Different compositions should be associated with different indications
- Today’s long-term clinical studies are based on 3Y-TZP zirconia, and report satisfying results for single, 3- or 4-unit FDPs on teeth
[1] Lava™
[2] MDP Monomer (10-Methacryloyloxydecyl dihydrogen phosphate)
Presentation figures
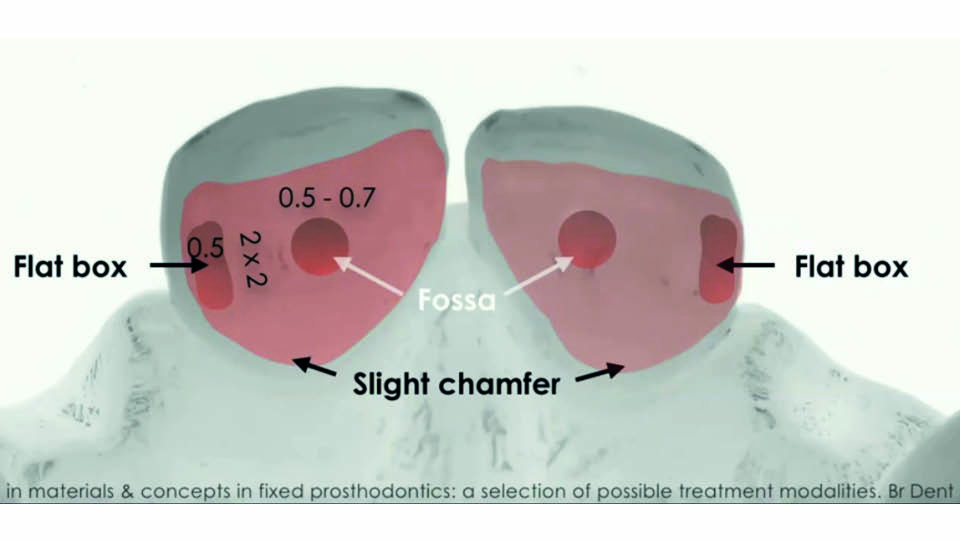
Fig 1: Preparation of abutment teeth
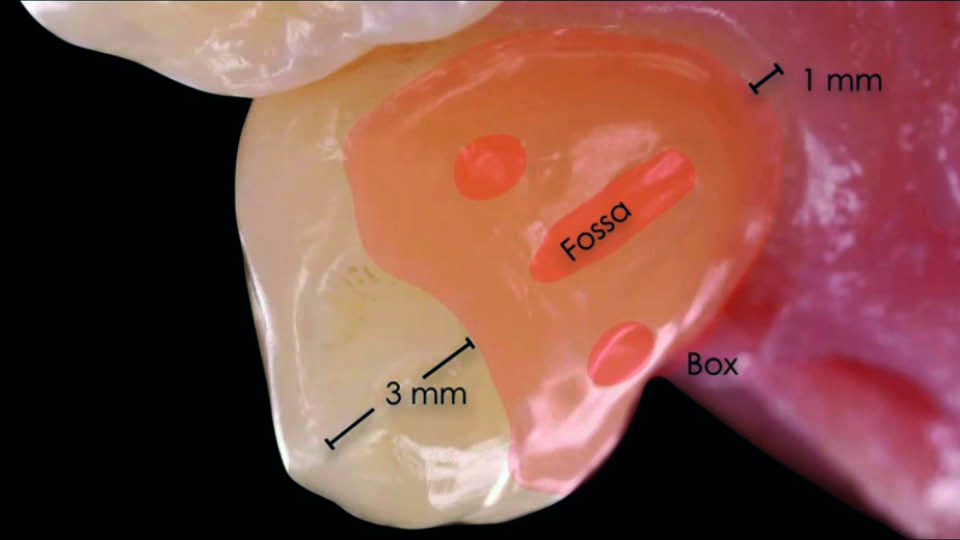
Fig 2: Adhesion area
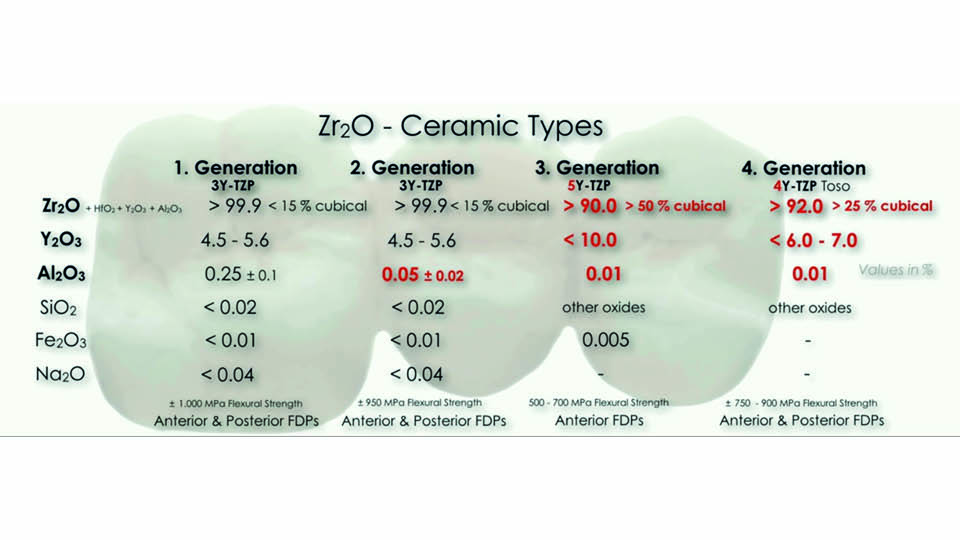
Fig 3: Evolution of zirconia ceramics
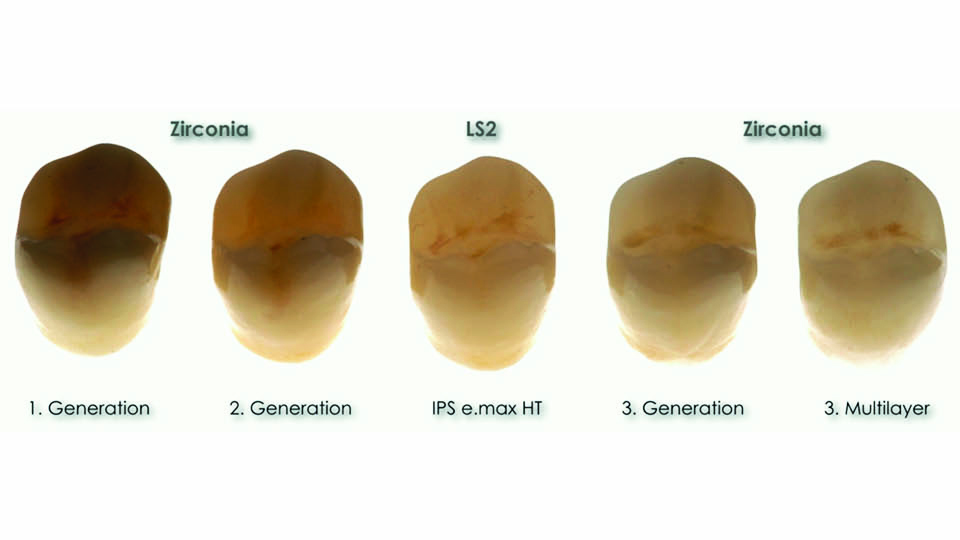
Fig 4: Monolithic translucent zirconia
References:
Beuer F, Schweiger J, Eichberger M, Kappert HF, Gernet W, Edelhoff D. High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings–a new fabrication mode for all-ceramic restorations. Dent Mater. 2009;25(1):121-8.
Edelhoff D, Stimmelmayr M, Schweiger J, Ahlers MO, Güth JF. Advances in materials and concepts in fixed prosthodontics: a selection of possible treatment modalities. Br Dent J. 2019A;226(10):739-48.
Edelhoff D, Liebermann A, Gütz JF. Randomized clinical study on metal- vs zirconia-based anterior two-wing resin-bonded fixed dental prostheses. 2019B (in preparation).
Gou M, Chen H, Kang J, Wang H. Antagonist enamel wear of tooth-supported monolithic zirconia posterior crowns in vivo: A systematic review. J Prosthet Dent. 2019;121(4):598-603.
Grohmann P, Bindl A, Hämmerle C, Mehl A, Sailer I. Three-unit posterior zirconia-ceramic fixed dental prostheses (FDPs) veneered with layered and milled (CAD-on) veneering ceramics: 1-year follow-up of a randomized controlled clinical trial. Quintessence Int. 2015;46(10):871-80.
Inokoshi M, Van Meerbeek B. Adhesively luted zirconia restorations: why and how? J Adhes Dent. 2014;16(3):294.
Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018;120(1):132-7.
Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51-5.
Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17(1):7-26
Preis V, Grumser K, Schneider-Feyrer S, Behr M, Rosentritt M. The effectiveness of polishing kits: influence on surface roughness of zirconia. Int J Prosthodont 2015;28(2):149-51.
Sailer I, Balmer M, Hüsler J, Hämmerle CHF, Känel S, Thoma DS. 10-year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J Dent 2018;76:32-9.
Schwindling FS, Waldecker M, Rammelsberg P, Rues S, Bömicke W. Tooth substance removal for ceramic single crown materials-an in vitro comparison. Clin Oral Investig 2019;23(8):3359-66.
Teichmann M, Wienert AL, Rückbeil M, Weber V, Wolfart S, Edelhoff D. Ten-year survival and chipping rates and clinical quality grading of zirconia-based fixed dental prostheses. Clin Oral Investig. 2018;22(8):2905-15.
Wei YR, Wang XD, Zhang Q, Li XX, Blatz MB, Jian YT, Zhao K. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J Dent. 2016;47:1-7.
Zhang Y, Lawn BR. Novel Zirconia Materials in Dentistry. J Dent Res. 2018;97(2):140-7.
Zirconia on implants
With the digital revolution comes a real ‘material revolution’, evidenced by the rapidly evolution of dental ceramics. Although zirconia has evolved a great deal, it is still not the ideal material: it has both advantages and disadvantages. In the last few years, partially-translucent and translucent zirconia have been added to the portfolio along with traditional zirconia. These are achieved by increasing the cubic phase. The bad news, however, is that this process decreases the flexural strength of traditional zirconia by up to the half.
There are different possibilities for using zirconia in the field of implant prosthodontics, such as (fig 5):
- zirconia abutments or zirconia cemented on titanium bases
- zirconia crowns or hybrid crowns
- fixed partial restorations with zirconia at the implant level or the abutment level
Zirconia abutments
It is widely recognised that for abutments, it is generally better to have a titanium base rather than a whole zirconia abutment. A recent systematic review (Naveau et al., 2019) reached the following conclusions:
- zirconia abutments show a 96% survival rate
- when peri-implant mucosa is thinner than 2mm, the aesthetic appearance of zirconia abutments is superior to that of titanium abutments
- when angulation is greater than 20º, titanium abutments are safer than zirconia abutments to reduce fracture risk (fig 6)
Zirconia crown
The problem is not in the frame, but in the ceramic veneering that – according to the literature – is prone to chipping. In general, zirconia crowns on implants show good prosthetic survival rates (Abou-Ayash et al., 2017).
Hybrid zirconia crown (zirconia-abutment-crown)
The weakest point is the bonded interface between titanium base and zirconia. Regarding this type of restoration, there are more questions than answers:
- what is the ideal height/configuration of titanium base?
- what influence does angulation have on resistance?
- what is the ideal luting cement/luting protocol?
- what is the long-term clinical performance?
Zirconia fixed partial dentures (FPDs)
The inherent problem here is that the 5-year fracture rate of veneering ceramics is 31%, twice that of zirconia prostheses on teeth (Saito et al., 2010). This may be due to the absence of damping, and proprioception in the case of implants.
Data about zirconia FPDs are under-reported in the literature. Concerning cantilevers, information about hybrid prostheses, or whether restorations should be at implant- or abutment-level, are not indicated.
Several solutions have been proposed to deal with high rates of fracture complications:
- a more anatomical core design (to better support the veneering ceramic)
- modifying the ceramic used for veneers: CAD-CAM fabrication, slow cooling approach, etc.
- not grinding the ceramics
Monolithic zirconia
Without veneers, the fractures disappear. First is the matter of antagonist wear, where the roughness value is the major impact factor, according to an in vitro study (Aldegheishem 2015). The greater the surface roughness, the greater the coefficient friction and the greater amount of wear in the antagonist. Therefore, post-sintering surface modifications of monolithic zirconia restorations should be avoided. Any occlusal adjustments should be followed by a thorough polishing sequence.
Full-arch zirconia fixed prostheses
The speaker presented a clinical case treated using a full digital workflow, involving a definite prosthesis made by monolithic zirconia only in the anterior group; the incisal edges of the buccal veneers were protected by the framework to prevent chipping.
The clinical outcome of full-arch zirconia prostheses was reviewed systematically (Bidra 2017). 42 out of 285 were found to have chipping (14.7%), and 4 had fractured or loose abutments (1.4%). Another study found that the five-year cumulative survival rate of 2,039 fixed full-arch zirconia prostheses was 99.3%, with a minimal technical complication (Bidra et al., 2018). Six fractures were recorded (0.29%) caused by inaccurate casts, reduced prosthetic space and adjacent implants positioned too closely. These results support the view that monolithic zirconia are an excellent choice for full-arch implant rehabilitation.
Another meta-analysis was recently performed comparing complete implant-supported prostheses on metal-ceramic, veneered zirconia and metal-resin compositions. Chipping rate was 8%, 15% and 22% respectively. De-cementation was also found to be an issue in metal-ceramic restorations (rate of 11%), but no abutment fractures were reported (Bagegni 2019).
An overview of the speaker’s clinical recommendations can be seen in figure 7.
Conclusions
- zirconia abutments show high survival rates
- clinical data about zirconia hybrid abutments and hybrid crowns is still lacking
- long-term data about single zirconia crowns and FPDs is limited
- there is also limited data about segmented zirconia full-arch prostheses
- prothesis fractures are mostly attributed to limited prosthetic space
- the main complication is chipping of the veneering ceramic
- monolithic zirconia offers enhanced mechanical properties, but further development is still needed to optimise aesthetics
Presentation figures

Fig 5: Different uses of zirconia
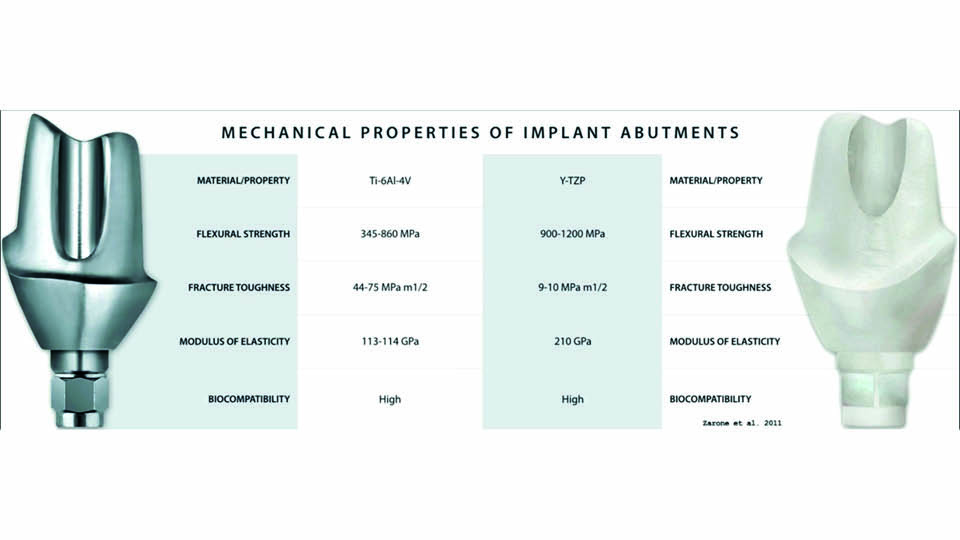
Fig 6
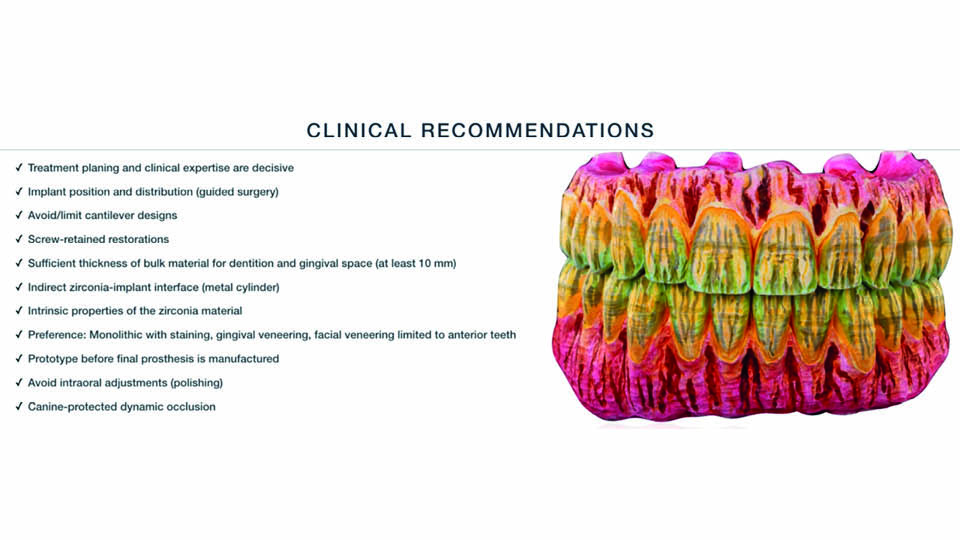
Fig 7
References:
Abou-Ayash S, Strasding M, Rücker G, Att W. Impact of prosthetic material on mid- and long-term outcome of dental implants supporting single crowns and fixed partial dentures: A systematic review and meta-analysis. Eur J Oral Implantol 2017;10 Suppl 1:47-65.
Aldegheishem A, Alfaer A, Brezavšček M, Vach K, Eliades G, Att W. Wear behavior of zirconia substrates against different antagonist materials. Int J Esthet Dent 2015;10(3):468-85.
Bagegni A, Abou-Ayash S, Rücker G, Algarny A, Att W. The influence of prosthetic material on implant and prosthetic survival of implant-supported fixed complete dentures: a systematic review and meta-analysis. J Prosthodont Res 2019;63(3):251-65.
Bidra AS, Rungruanganunt P, Gauthier M. Clinical outcomes of full arch fixed implant-supported zirconia prostheses: A systematic review. Eur J Oral Implantol 2017;10 Suppl 1:35-45.
Bidra AS, Tischler M, Patch C. Survival of 2039 complete arch fixed implant-supported zirconia prostheses: A retrospective study. J Prosthet Dent. 2018;119(2):220-4.
Naveau A, Rignon-Bret C, Wulfman C. Zirconia abutments in the anterior region: A systematic review of mechanical and esthetic outcomes. J Prosthet Dent 2019;121(5):775-81.
Saito A, Komine F, Blatz MB, Matsumura H. A comparison of bond strength of layered veneering porcelains to zirconia and metal. J Prosthet Dent. 2010;104(4):247-57.



